BCG Vaccine: Information for Health Professionals - HE2204
Information for lead maternity carers and other health professionals about which children should be offered the BCG vaccination, the vaccine's efficacy and possible side effects.
The full resource:
Information for health professionals
This resource explains who should and shouldn’t have the BCG vaccine, when the vaccine should be given, and who can give the vaccine. It also describes the vaccine's efficacy and possible side effects. See below for sources of more information about tuberculosis (TB) and the BCG vaccine.
PLEASE NOTE:
- You should screen all women during pregnancy to assess whether their baby is at increased risk of catching TB.
- BCG vaccine is free for all babies and children less than 5 years who are at increased risk of catching TB.
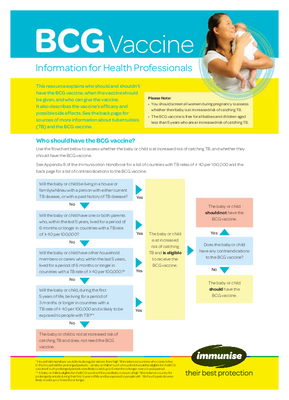
Who should have BCG vaccine?
Use the flowchart below to assess whether the baby or child is at increased risk of catching TB, and whether they should have the BCG vaccine.
See Appendix 8 of the Immunisation Handbook for a list of countries with TB rates of ≥ 40 per 100,000 and below for a list of contraindications to the BCG vaccine.

* Household members would include regular visitors from high TB incidence countries who come to live in the household for prolonged periods – a baby or child in such a household would be eligible for BCG vaccine if such prolonged periods were likely to add up to 6 months or longer over a 5-year period.
** A baby or child is eligible for BCG vaccine if they are likely to stay in a high TB incidence country for prolonged periods during their first 5 years of life and be exposed to people with TB, if such periods were likely to add up to 3 months or longer.
BCG vaccine contraindications
BCG should not be given to babies or children:
- receiving corticosteroids or other immune-suppressive treatment, including radiotherapy
- suffering from malignant conditions such as lymphoma, leukaemia, Hodgkin's disease or other tumours of the reticulo-endothelial system
- in whom an immune compromising disease is known or suspected, such as individuals with hypogammaglobulinaemia*
- known or suspected to be inected with HIV, including neonates with suspected HIV infection (ie, if the mother has HIV**)
- with a positive Mantoux test or positive Interferon Gamma Release Assay (IGRA)
- with a significant fever
- with generalised septic skin conditions (for eczema, choose a site free from lesions)
- living in a household where a possible case of active TB is being investigated. (The baby or child can receive the BCG vaccine if testing confirms they are not already infected with TB.)
NOTES:
* Primary immune deficiencies in children are often not detected until after the first few weeks of life (ie, after BCG vaccine is given). A family history of immune deficiency should be sought and, if present, discussed with a paediatrician before vaccination.
** Neonates whose mothers have HIV infection must not be given BCG (or any other live vaccine) until the baby has been shown to be HIV negative, which can only be confirmed at 12–18 months of age. Discuss with the child's paediatrician prior to vaccinating.
When to give BCG vaccine
- Neonates should receive the BCG vaccine before they leave hospital, or as soon as possible following discharge from hospital.
- If the baby or child missed vaccination at birth, they can be vaccinated anytime up to five years of age. If older than six months of age, a pre-vaccine Mantoux test is required to detect if the baby or child is already infected with TB.
Who can give the BCG vaccine?
Only gazetted BCG vaccinators are able to administer BCG vaccine. Contact your local public health service to find out who your local gazetted vaccinators are, and the requirements for becoming gazetted.
BCG vaccine efficacy
While BCG vaccine does not prevent TB infection, it does help protect against severe or disseminated forms of childhood TB, particularly miliary and meningeal disease. Evidence suggests that BCG vaccine is less effective in older children and adults. Therefore, the BCG vaccine is recommended and funded for those babies and children less than five years of age who are at increased risk of TB.
Expected responses and adverse events
Most babies and children develop local reactions to BCG vaccine, followed by healing and scar formation within three months. Many develop low-grade adenitis that can take several months to resolve. Refer to the Immunisation Handbook for rarer complications. Report adverse events to the Centre for Adverse Reactions Monitoring (CARM).
More information
For Health Professionals
- The Ministry of Health
- The Tuberculosis chapter and Appendix 8 of the Immunisation Handbook
- Guidelines for Tuberculosis Control in New Zealand 2010
- The Tuberculosis chapter of the Communicable Disease Control Manual
- Your local Medical Officer of Health, gazetted BCG vaccinator or Public Health Service
- The Immunisation Advisory Centre - www.immune.org.nz or 0800 IMMUNE (0800 466 863).
For Parents, Family and Whānau
- BCG vaccine information for parents (Code HE2205, plus community language translations)
- Minstry of Health - Tuberculosis