More about Breast Screening and BreastScreen Aotearoa
This resource is currently under review and is available as an online resource only until the review is completed.
The full resource:
Detailed information about the breast screening programme and how regular mammograms help in the early detection of breast cancer.
Early detection is your best protection
Did you know that
- Free breast screening for women aged 45–69 years is provided by the national breast screening programme, BreastScreen Aotearoa.
- The aim of breast screening is to find very small cancers before a lump can be felt in the breast. Early treatment has the best chance of success.
- Breast cancer is the most common cancer in New Zealand women.
- The risk of developing breast cancer increases with age. Breast cancer is uncommon in women under 50.
- For older women, breast screening using mammography (breast X-rays) followed by appropriate treatment is the best way of reducing the chance of dying from breast cancer.
Mammography screening:
- detects cancer but cannot prevent it
- does not guarantee that cancer is not present
- reduces the risk of dying from breast cancer but does not eliminate it.
About this booklet
This booklet provides information to help women decide about whether to take part in the national breast screening programme, BreastScreen Aotearoa. It is written specially for women who want more information than is contained in pamphlets about the programme.
The booklet outlines the benefits, limitations and risks of breast screening at different ages. It discusses what it means to enrol in the programme. It provides information about breast cancer and BreastScreen Aotearoa.
If you don’t want to read the whole booklet now, you can keep it to refer to in the future.
Information in the booklet can also be shared with your partner, whānau and family.
You can take the booklet to your usual health care provider to discuss it with them. If you want to find out more about anything in this booklet, you can talk to your doctor or contact one of the groups listed under Where to go for further information.
Information about the programme is also available on the BreastScreen Aotearoa website.
Contents
About this booklet
Introduction
Section 1: Breast screening
What are mammograms?
What is breast screening
About the normal breast
Having a mammogram
Section 2: Deciding about breast screening
Benefits and risks of breast screening
Limitations and risks of breast screening
Section 3: Results of mammograms
Results of mammograms
Following up abnormal mammograms
Treatment options
Section 4: Breast cancer
Breast cancer in New Zealand
What causes breast cancer?
Family history
Section 5: BreastScreen Aotearoa
BreastScreen Aotearoa
Consumer rights in BreastScreen Aotearoa
References
Where to go for further information
Glossary
Index
Acknowledgment
Introduction
Breast cancer is an important health problem for New Zealand women. Unfortunately, there is little women can do to prevent breast cancer. At present, for older women, breast screening using mammography (breast X-rays) followed by appropriate treatment is the best way of reducing the chance of dying from breast cancer. It also increases the chance that women with breast cancer can be offered breast-conserving surgery, in which only part of the breast is removed.
BreastScreen Aotearoa is the national programme that offers free breast screening to women aged 45–69. Breast screening provides benefits in reducing deaths, but it may also cause harm. BreastScreen Aotearoa ensures services in the programme are of a high quality so that the benefits outweigh the harm.
Many women are unsure of their risk of breast cancer and of what mammography can offer. Women tend to overestimate their risk of breast cancer. They may also overestimate the benefits of breast screening.
It is important that women make an informed decision about whether to enrol in the BreastScreen Aotearoa screening programme. This booklet will provide information to help you make that decision.
The booklet is in five sections:
Section 2: Deciding about breast screening
Section 3: Results of mammograms
Section 5: BreastScreen Aotearoa
Glossary
In this booklet we have included some technical words you might hear during breast screening. A glossary is provided to explain the meaning of technical words used in this booklet. Words you will find in the glossary are highlighted like this the first time they appear. You can look in the glossary any time you come across a word that is unfamiliar.
Quality Standards
BreastScreen Aotearoa has set a number of quality standards for the programme. Providers of breast screening services are required to maintain these standards.
Some of the standards are printed throughout the booklet in boxes like this. The complete standards can be seen on the BreastScreen Aotearoa website at www.nsu.govt.nz The standards are updated from time to time. See the website for the latest version.
Section 1
Breast screening
What are mammograms?
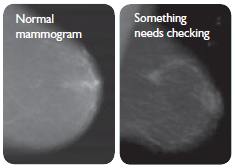
Mammograms are X-rays of the breast. They provide a picture of the tissue inside the breast. Mammograms can show up abnormal-looking tissue in the breasts.
A mammogram on its own is not enough to show if abnormal-looking tissue is definitely cancer. Other tests are needed to diagnose or identify what the mammogram has found (more information under Methods for diagnosing breast cancer).
What is breast screening?
The aim of mammography screening is to find very small cancers before a lump can be felt in the breast. Treating breast cancer when it is small gives a woman a better chance that her treatment will be successful. It also increases her chance of having breast-conserving treatment.
Breast screening aims to find cancers – it does not prevent cancer occurring.
By taking part in regular mammography screening from the age of 45, a woman reduces her risk of dying from breast cancer.
Mammography screening cannot stop every woman with breast cancer from dying. Even when small, some breast cancers may already have spread to other parts of the body.
Some breast cancers will be missed by screening and a few types of breast cancer are difficult to detect on mammograms.
Screening does not give a guarantee, but it does reduce the risk of dying from the most common cancer in women.
About the normal breast
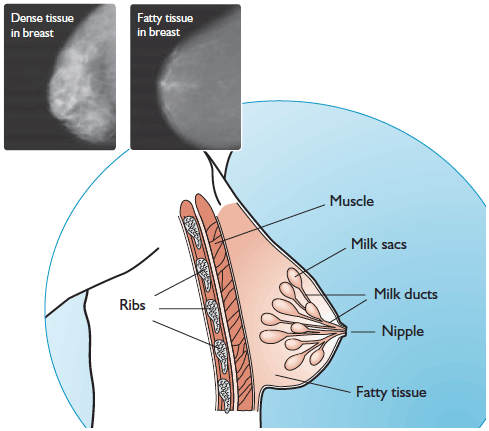
The breast is made up of tissue that provides support for sacs (called lobules) for making milk, and tubes (called ducts) for taking the milk to the nipples when a woman feeds her baby (see diagram). There is fat in the support tissue, and this can increase and decrease with weight gain and loss.
About the age of 50, women go through the ‘change of life’ or menopause. Before menopause, women’s breasts contain more dense (glandular) tissue. This makes mammograms harder to ‘read’ and less accurate. After menopause, the dense glandular tissue is increasingly replaced by fat. This makes the mammograms easier to read and more accurate.
This is why the information about the benefits and risks of mammography screening is given separately for women over 50, and under 50, in this booklet.
Diagram showing the internal structure of the female breast, and images of mammograms illustrating the difference between dense and fatty tissue in breasts
Having a mammogram
How often do you have mammograms?
Women who enrol in BreastScreen Aotearoa are invited to have a mammogram every two years from the age of 45–69 years.
Women who are eligible for BreastScreen Aotearoa
Once you decide to enrol in BreastScreen Aotearoa, you can have a free screening mammogram every two years if you meet all the following:
- are aged 45–69 years
- have no symptoms of breast cancer
- have not had a mammogram in the last 12 months
- are not pregnant or breastfeeding
- are eligible for public health services in New Zealand.*
How do you join BreastScreen Aotearoa?
There are several ways of enrolling with BreastScreen Aotearoa.
- You can enrol yourself by phoning 0800 270 200.
- Your doctor may invite you to take part.
- You can ask your doctor to refer you.
- Your Māori or Pacific primary health care or health promotion provider can enrol you.
- You can enrol on the BreastScreen Aotearoa website.
There is more information about what it means to enrol in BreastScreen Aotearoa in Section 5.
Where do you go for breast screening?
BreastScreen Aotearoa provides clinics for breast screening all around New Zealand. Some of these are in the community, and some are at public hospitals. As well, BreastScreen Aotearoa has mobile screening units that are available in rural and some urban areas.
To find out more:
- ring 0800 270 200
- visit the website to find out what is available near where you live.
Preparing for your mammogram
When you go for your mammogram, you will be given a private place to change. You will be provided with a gown to wear if you want to.
- Wear a top with pants or skirt as you will need to undress from the waist up.
- Don’t use talcum powder, creams or deodorant on the day. These can make the mammogram difficult to read.
- Bring your reading glasses as you may need to fill in a form or read something.
- Bring any previous mammograms that you have. If the programme has these for comparison when reading your mammogram, the chance of a false positive (normal mammogram read as abnormal) is more than halved. There is more information about this under False positive results.
How is it done?
A mammogram is done by a health professional called a medical radiation technologist or MRT (formerly called a radiographer). The MRT is usually a woman.
She will position one breast at a time between two plates on the X-ray machine. This flattens the breast and holds it still. This is necessary to give a good image of the breast and reduce the radiation dose. Two views are taken of each breast.
The mammograms are films that look like the negatives of photos. Specialist doctors called radiologists ‘read’ these films. This means they put them on a lighted box and study them carefully for areas that look abnormal. Abnormal-looking areas show up as white areas on the films. Many harmless conditions can also show up on mammograms.
When reading mammograms, previous mammograms are obtained, wherever possible, for comparison ...
Films are read independently by two radiologists, both of whom meet the radiology training requirements as specified ...
Does having a mammogram hurt?
Most women say it is uncomfortable. Some women find the procedure painful. If you feel pain, tell the MRT carrying out the mammogram. Some women also have pain or soreness after the mammogram. A few women have some bruising after the mammogram. Women who find mammography painful are advised to take a mild over-the-counter painkiller 30 minutes before the mammogram. Mammography does not harm the breasts.
Women with large breasts
MRTs take particular care when taking mammograms for women with large breasts to ensure they get good images. It can be more difficult to position the breasts, and the MRT is careful not to damage the skin or expose the breasts to too much radiation. The MRT can use larger films to get good images. It can take longer to take the mammograms for women with large breasts.
Women with small breasts
MRTs are trained to be able to take mammograms regardless of the size of a woman’s breasts. Women may feel discomfort as the breast is compressed, and some women may feel pain. Pain is no more likely for women with small breasts than for women with larger breasts. The size of a woman’s breasts does not affect her risk of breast cancer, and mammography is as effective for women with small breasts as for other women. There is always a small amount of tissue on the chest wall that cannot be seen on a mammogram, but this is the same for all women, regardless of breast size.
How long does a visit take?
You should allow about 30 minutes for the visit. The actual mammogram only takes a few minutes.
How much will it cost?
BreastScreen Aotearoa is free, including screening and any associated follow-up tests. Treatment for breast cancer is free in public hospitals. Travel assistance for women from rural areas to attend assessment clinics can be discussed with the breastcare nurse.
What you can do if you need more information or support
Going for a mammogram and waiting for results can be worrying. Women who are asked to come back for more tests are often anxious about what this means, even though the chance of being told they have cancer is only about 1 in 10. You and your family/whānau can get support from the breastcare nurse who is part of the screening service.
The breastcare nurse is a registered nurse who has had special training about breast cancer and women’s needs as they take part in breast screening. She can provide women with information, education, counselling and support at any time during screening and assessment.
Can you bring a friend for support?
You are welcome to bring a friend or whānau/family members with you throughout screening and assessment. They can be with you except where the privacy of other women is affected. They may be asked to leave the room during the actual mammogram because of the radiation risk.
Technical repeat mammograms
Some women are called back for more X-rays because the first ones were not of good enough quality to be clearly read. In BreastScreen Aotearoa, less than 1 percent of women who have mammograms at a fixed unit and about 4 percent at a mobile unit are recalled for more X-rays.
Women with possible symptoms of breast cancer
BreastScreen Aotearoa offers mammography screening to women with no symptoms of breast cancer. Mammography alone is not sufficient to diagnose the cause of breast symptoms such as a new lump, nipple change or skin puckering. Women with such symptoms will be referred to their doctor, who can arrange for them to go to a specialist or outpatient service for diagnosis.
Women who have had breast cancer
For the first five years after a diagnosis of cancer, a woman will need close follow-up by a doctor. After this, women who have had breast cancer are able to enrol or re-enrol in BreastScreen Aotearoa. This includes women who have had a mastectomy, who can have screening of the other breast.
Women with a disability
Women are usually asked when making an appointment if they have any special needs due to a disability. If you are not asked, tell the person making the appointment about your needs. This enables the service to plan for the visit, including allowing more time. The quality of the mammograms can be checked before the woman leaves. This is not possible at a mobile unit. Although mobile units have a wheelchair hoist, women with physical disabilities are encouraged to attend a clinic because clinics are better able to provide access, allow more time and accommodate carers.
Women with breast implants
Some women who come for screening have implants in their breasts. Screening is more difficult for women with breast implants, and extra views need to be taken. Even so, some parts of the breast may not be seen. Women need to inform the service at the time of making an appointment if they have breast implants. The appointment needs to be longer. It is important to attend a fixed site rather than a mobile unit so the mammograms can be processed immediately to check the quality.
Women with breast implants will be asked to sign a special consent form. This points out that cancer is more likely to be missed in women with implants. There is also a very small chance the implant could be damaged during the mammogram. The mammogram may sometimes show damage or breaking of the implant.
Women on hormone replacement therapy (HRT)
Some women are using hormone replacement therapy (HRT), and you will be asked about this when you come for screening. Using HRT can make breast tissue more dense, making mammograms harder to read. Because of this, women who use HRT are more likely to be recalled for abnormal mammograms when there is actually nothing wrong. Women using HRT are also more likely to have breast cancers missed. For more information on HRT go to www.nzgg.org.nz or www.womens-health.org.nz
What happens when you turn 70?
If you are aged 70 or over, you cannot have free mammograms with BreastScreen Aotearoa. There is very little evidence of a benefit from screening women over 70.
Breast cancer that occurs in women with a family history of breast cancer usually does so before the age of 70. If you are concerned about your risk of breast cancer, you can discuss this with your doctor.
Section 2
Deciding about breast screening
Benefits and risks of breast screening
When you are deciding whether to take part in breast screening, you will want to weigh up the benefits and risks.
The first part of this section looks at the benefits of breast screening. It is divided into two parts:
- the benefits of breast screening for women over 50
- the benefits of breast screening for women under 50.
The benefits of breast screening are not the same for these two age groups.
Breast screening is less effective in younger women, so they need different information.
Benefits of breast screening for women over 50
The risk of breast cancer increases as women get older. Around three-quarters of breast cancers are diagnosed in women 50 years and over.
Mammograms will find about 85–90 percent of all unsuspected cancers in women over 50. A number of studies have shown that women in this age group benefit from having regular screening mammograms.
To prevent one breast cancer death, 1430 women aged 50–69 years need to have a mammogram.
| Women 50 years and over | Without screening | With regular 2-yearly screening | Percentage reduction in risk with screening |
|---|---|---|---|
| Chances of getting breast cancer by the age of 70 | 1 out of 17 women | 1 out of 17 women | No reduction |
| Chances of dying from breast cancer by the age of 70 | 1 out of 70 women | 1 out of 100 women | 30 percent reduction |
Diagram illustrating statistics on women aged 50–69 who have breast screening every two years for 20 years
These numbers have been estimated by applying the results of overseas studies to New Zealand.
Benefits of breast screening for women under 50
About 20 percent of cases of breast cancer are diagnosed in women in their 40s. Mammography screening can detect cancers in these younger women, but they gain less benefit from screening than older women and there are more risks.
There are a number of reasons for this.
- Mammograms are less reliable in younger women. Mammograms are more effective on fatty breast tissue. Younger women usually have dense breast tissue with less fat. This can make mammograms more difficult to read. As a result, some cancers are not detected. Up to 25 percent of invasive breast cancers are not detected in women in their 40s, compared with 10 percent in women in their 50s.
- Younger women are also more likely to have false positive results. These are abnormal-looking areas on mammograms that turn out not to be cancer (more information under False positive results).
- The radiation risk from mammograms may be greater for women in their 40s (more information under Radiation risk).
- Breast cancer may be subtly different in women under 50 compared with that in older women. The disease might progress more rapidly in women before menopause.
There are different ways of expressing the effectiveness of breast screening to women in this age group.
- Women in their 40s who have regular mammograms as part of a screening programme reduce their chances of dying from breast cancer by about 20 percent or less.
- To prevent one breast cancer death, 1800 women in their 40s need to be invited to take part in screening for 14 years.
| Women 45–49 years | Without screening | With regular 2-yearly screening | Percentage reduction in risk with screening |
|---|---|---|---|
| Chances of getting breast cancer by the age of 50 | 1 out of 100 women | 1 out of 100 women | No reduction |
| Chances of dying from breast cancer by the age of 50 | 1 out of 300 women | 1 out of 400 women | 20 percent or less reduction |
Diagram illustrating statistics on women aged 45 who have breast screening every two years for five years
These numbers have been estimated by applying the results of overseas studies to New Zealand.
The evidence that mammography screening reduces deaths from breast cancer in women in their 40s is weaker than for women over 50. This is why most countries with breast screening programmes do not invite women in their 40s.
The advantages and disadvantages of taking part in screening before the age of 50 are summed up in the table below.
| On the plus side | On the minus side |
|---|---|
| Both reduce the risk of dying from breast cancer, but the reduction is smaller for women under 50. | Weaker evidence of benefit |
| Smaller reduction in risk of dying | |
| Less accurate at finding cancers | |
| Fewer cancers found | |
| More false positives | |
| Greater likelihood of over-diagnosis | |
| Greater risk of cancers caused by X-ray radiation |
Studies have not shown a clear advantage of annual rather than two-yearly mammograms for women in their 40s.
Limitations and risks of breast screening
A mammogram is not a perfect test. Cancers will be missed in some women. On the other hand, the vast majority of women who take part in breast screening do not have breast cancer. These women do not gain a benefit from breast screening, but they can be harmed. There are limitations and risks to women in mammography screening. These are discussed below.
False positive results
This means a woman is told her mammogram looks abnormal, but further tests show that she doesn’t have cancer. These further tests usually include more mammograms and ultrasound examination. In some cases, a biopsy is needed to take breast cells or tissue for testing. In BreastScreen Aotearoa about 8 percent of women having a first screening mammogram and 3 percent who have subsequent mammograms will have a false positive. These tend to be higher in younger women. For women who have regular mammograms over some years, the risk of a false positive result accumulates. After 10 years, about a quarter of all women having screening mammograms two-yearly will have had a false positive and about 1 in 20 will have had a needle biopsy.
Cancers that are found after a normal mammogram
 Cancers that are diagnosed within two years of a woman being returned to screening are called interval cancers. This can happen for a number of reasons.
Cancers that are diagnosed within two years of a woman being returned to screening are called interval cancers. This can happen for a number of reasons.
- Some cancers do not show up on a mammogram. (This is more likely in women before the menopause, who often have dense breast tissue.)
- The radiologists looking at the mammogram may miss the cancer. (This will happen sometimes, no matter how experienced the radiologists are.)
- Sometimes a fast growing cancer will develop.
A woman who notices an unusual change in her breast between mammograms should get this checked by her doctor even if she has recently had a normal mammogram.
Radiation risk
Mammograms are X-rays and use radiation. Radiation increases the risk of breast cancer developing. For a woman attending breast screening every two years from the age of 50, the risk of dying from a breast cancer caused by radiation is very small. It is estimated to be 10–50 per million screened women.
Younger women are more sensitive to the risk of developing a radiation-induced cancer from mammography screening. Although the risk is small, it does increase the earlier a woman starts mammography and the shorter the screening interval.
Women with larger than average breasts may receive larger than average doses of radiation.
BreastScreen Aotearoa monitors the equipment used to take mammograms to ensure radiation is kept to a minimum.
Possible over-diagnosis and over-treatment
This means finding and treating conditions that may never have caused a woman problems had they not been detected by screening.
Mammography can detect some breast conditions that are not well understood. There is uncertainty about whether they will progress to cancer and what the best treatments are. Sometimes the abnormal tissue can be spread through one breast or, rarely, through both breasts. This means that it can only be removed by complete removal of the breast or breasts. Women in this situation sometimes have more extensive surgery than women with invasive cancer. One of the conditions is called ductal carcinoma in situ (DCIS). There is more about this under Ductal carcinoma in situ or DCIS.
Over-diagnosis and over-treatment are estimated to account for between 5 and 25 percent of cancers detected by breast screening. The risk of over-diagnosis may be greater in women under 50 than in women over 50.
Scarring
Excision or open surgical biopsies cause scars. Sometimes these are noticeable, and occasionally they may also decrease the ability to detect cancer in the future.
Section 3
Results of mammograms
Results of mammograms
When and how will you get your results?
You will usually get your results within two weeks of having the mammogram.
Your doctor can also be told the result if you agree.
Most women’s results will be normal.
What will the results of the mammogram say?
Normal results
If nothing abnormal was found on your mammogram, you will receive a result letter that will say:
‘We are pleased to inform you that your mammogram has been reviewed and reported by two qualified radiologists and they found no evidence of breast cancer.’
This means that you are at low risk of having breast cancer diagnosed in the next two years. The letter will not tell you if any harmless conditions were found on the mammogram.
Within two years of your last mammogram, you will receive an appointment from BreastScreen Aotearoa.
Even if you have had a normal mammogram, you need to be aware of any changes to your breasts before your next mammogram is due. There is more about this under Breast awareness.
If you move to another region in the meantime, you need to notify the BreastScreen Aotearoa service you attended so they can send your mammograms to the service nearest you, who will invite you for your next mammogram.
Mammograms are kept for 10 years after a woman’s last visit to BreastScreen Aotearoa.
Abnormal results
If anything abnormal looking is found on your mammogram, you will be telephoned by the breastcare nurse from the service you attended and asked to attend an assessment clinic. You will also be sent information about what happens at assessment. About 9 percent of women attending for their first mammogram and 4 percent having subsequent mammograms will be asked to attend an assessment clinic.
An abnormal result does not necessarily mean you have cancer. About 9 of the 10 who are recalled will not have cancer. This means that only 1 in 10 women who are recalled will actually have cancer. However, many women feel anxious while waiting to attend the assessment visit and some women take a while to get back to normal. You might find it helpful to talk to your husband, partner, family members or friends. You can also talk to the breastcare nurse or your doctor.
Following up abnormal mammograms
What happens at the assessment clinic?
The assessment visit is to make a diagnosis. Further tests will be done to find out what has caused the abnormal look of the mammogram. Some harmless conditions show up on mammograms. Sometimes the only way to distinguish harmless conditions from cancer is to take further tests from the abnormal-looking area.
Assessment visits vary in length. For some women it may take only an hour; others will spend half a day or more. You may need to plan to be away for a whole day and make other arrangements for children, work or other commitments. The assessment is made by a multidisciplinary team of expert people. The team is made up of a breastcare nurse, an MRT, a radiologist, a pathologist and a surgeon. The nurse’s main role is to support and inform the woman and her friends, family or whānau members.
Ninety percent of women are offered an assessment appointment within 15 working days of their final screening mammogram.
The woman’s concerns regarding the assessment procedure, or any other related issues, are discussed and addressed in a manner that ensures the privacy of the individual and any relevant parties.
The breastcare nurse works as a member of a multidisciplinary team in partnership with women, their families and whānau to empower each woman to make informed choices and optimise her health and wellbeing.
Methods for diagnosing cancer
A number of tests are available to find out whether the abnormal- looking area of the mammogram is cancer or not. You might have one, two or several tests. The staff at the assessment clinics try to keep tests to the minimum. Two-thirds of recalled women only have more mammograms and an ultrasound scan. Only one in three women recalled will need a biopsy. At the assessment clinic, the staff will discuss with you the tests you are likely to need.
The assessment tests may include:
- Clinical breast examination – this involves looking at and feeling the breast.
- More mammograms to magnify a small area or look at it from a different angle.
- Ultrasound scan – a device is passed over the skin of the breast. High-frequency sound waves show whether a lump is a harmless cyst or something else. Not all conditions can be detected by ultrasound.
-
Needle biopsy – there are three different types of needle biopsy:
- fine needle aspiration biopsy (FNA) or
- core biopsy or
- vacuum-assisted biopsy (such as Mammotome).
If you need a needle biopsy, usually only one type is required.
Usually a fine needle, core or vacuum-assisted biopsy is performed using ultrasound or X-ray guidance to show where the abnormal tissue is.
The BreastScreen Aotearoa goal is that 90 percent of cancers are diagnosed by a needle biopsy, to avoid surgical biopsies.
Types of needle biopsies
Fine needle aspiration biopsy (FNA)
A fine needle is used to remove some cells from the suspicious area. Local anaesthetic to numb the area may not be necessary as the biopsy needle is very thin. The cells that have been removed are examined under a microscope by a pathologist.
Core biopsy
Local anaesthetic is given, then a slightly larger needle is used to remove a small core of tissue. The tissue sample is examined by a pathologist.
Vacuum-assisted biopsy, such as Mammotome
Under local anaesthetic, a probe is inserted under the skin and tissue is drawn out using gentle vacuum suction and a larger core biopsy needle.
A marker may be left in the breast tissue to show where the abnormal area was. This means that the surgeon can find the area again in case further surgery is needed.
- Excision or open surgical biopsy – this involves partial or total removal of the abnormal area. Only a small number of women require an open surgical biopsy. Open biopsies are performed when the needle biopsy has not given a clear result. It would not be done at your first assessment visit. Another date would be booked for this procedure. Usually a general anaesthetic is given when an open surgical biopsy is done. You will usually only stay in hospital for the day or for one night. The programme tries to keep open biopsies to a minimum. In BreastScreen Aotearoa about 2 in 1000 women screened have an open biopsy.
- Wire localisation open biopsy – this is used if abnormal tissue cannot be felt. A very fine wire or carbon marker is inserted into the area under X-ray or ultrasound guidance. A local anaesthetic is used for this. With the wire in place, the woman is taken to the operating theatre. While she is under local or general anaesthetic, the surgeon makes an incision and removes the tissue around the wire.
Open surgical biopsies should be performed by the surgeon who will be responsible for ongoing surgical management, should cancer be diagnosed.
Open biopsies should be 3.5 or less per 1000 women screened in the first ever round of screening, and 1.6 or less per 1000 women screened in subsequent rounds of screening.
Ninety percent of women requiring open surgical biopsy should have their operations performed within 15 working days of being notified of the need for this operation.
The adverse impact of diagnostic surgical biopsy on breast appearance, contour or shape shall be minimised.
Where a marker is to be left for this or other reasons, these must be explained to the woman and informed consent must be obtained.
When will you receive your assessment results?
You will be given provisional results at the assessment clinic or you will be told when to expect them.
Wherever possible, provisional results are to be given on the day of assessment.
Final results are only communicated to women after all clinical review processes are completed (that is, after the multidisciplinary meeting). The method and timeframe of result notification is discussed with the woman at the completion of her assessment visit.
Where the result of the assessment is ‘no evidence of cancer’, eligible women are placed on the routine re-screen list.
Time taken from final diagnostic needle biopsy to reporting results to the woman – 90 percent of women receive results within 5 working days of final diagnostic needle biopsy.
What will the assessment results show?
The biopsy results will be normal for most women. They will return to routine screening and receive another invitation in two years’ time. In about 10 percent of cases, the biopsy result will show an invasive cancer or an abnormal condition that could progress to cancer.
Women with a diagnosis of cancer will be given information about where and when they can get treatment. Then they will be referred to the treatment service they choose or they can discuss with their doctor what to do. Women with an abnormal condition that could progress to cancer will also receive advice about their options. Not all of these conditions will inevitably develop into invasive cancer. The most common is ductal carcinoma in situ (DCIS). This is discussed in more detail below.
Treatment options
Where can you go for treatment?
Treatment for breast cancer is available free in public hospitals and clinics. Some treatments are available in the private sector, but others, particularly radiotherapy, are not. There is a cost to the woman for private treatment. She may be able to claim some or all of this if she has medical insurance.
Women need to take time to consider which treatment option will suit them best. Although prompt treatment is important, the treatment of breast cancer is not usually a medical emergency. The surgeon and breastcare nurse can talk to you about how much time you have to make up your mind. You can change your mind about the type of treatment you have right up to the time of the surgery.
In BreastScreen Aotearoa, members of the multidisciplinary assessment teams, for example, a breastcare nurse, can provide information about treatment and support options.
There is also a booklet, Treatment Services and Support for Women with Breast Cancer, that is given to all women with cancer by the assessment team.
What treatments are available?
The treatment that is offered depends on the type, size and position of the breast cancer, whether it has spread, the woman’s age and her general health. For women with DCIS alone, the treatment options will be different. There is more on this under Ductal carcinoma in situ or DCIS.
There are two main options for the treatment of breast cancer.
- Surgical removal of the lump and an area of tissue around it, also called lumpectomy, wide local excision, partial mastectomy or breast-conserving surgery. Surgery is usually followed by a course of radiation therapy or radiotherapy (X-ray treatment). The course of radiotherapy can take up to six weeks, with treatment four to five times a week. This is to destroy any cancer cells still present in the breast. Many women continue their employment during this time, although radiotherapy can make you tired. If you live a long way from a cancer treatment centre, you will need to stay close to where you receive your treatment. Treatment centres can arrange subsidised or funded accommodation for you and a support person as well as a travel allowance to go home at weekends if you want to.
- Mastectomy or removal of the whole breast including some skin and the nipple. The chest muscles are not removed. Some women who have a mastectomy also have radiotherapy. In BreastScreen Aotearoa about 40 percent of women diagnosed with cancer have a mastectomy.
Long-term survival is the same for both these treatments.
With both of these options some of the lymph nodes are usually removed from the armpit to check if the cancer has spread into the lymphatic system, the body’s drainage system. You may be offered sentinel node biopsy. This involves removing one, two or a few lymph nodes. You can discuss this with the surgeon.
If the cancer has spread to the lymph nodes, further treatment may be offered in the form of chemotherapy or treatment with a hormone drug or both.
Many women whose lymph nodes are clear may still be offered hormone treatment and some may still have chemotherapy.
Reconstruction
Women who are having a mastectomy may be offered a breast reconstruction at the time of the operation or at some later time, using skin, muscle and fat from their abdomen or back. Sometimes breast implants are suggested. Reconstruction involves major surgery. Many public hospitals offer reconstruction. It is also available in the private sector but is costly. If interested, a woman should ask about it. The Cancer Society has an Australian booklet that discusses the options, called Breast Reconstruction: Your Choice: A Guide for Women Considering Breast Reconstruction after Mastectomy.
For further information on implants, ask the doctor treating you or the breastcare nurse. Other information may be available from your local Cancer Society or a local women’s health group.
Where can you get more information about treatments?
More information is available from your local Cancer Society. You can ask for their booklet Breast Cancer Te Mate Pukupuku o ngā Ū: A Guide for Women with Breast Cancer in the Understanding Cancer series.
There are also helpful websites listed under Where to go for further information.
What happens after treatment?
After treatment for breast cancer, you should receive close follow-up care from a doctor. This follow-up usually includes annual mammograms, which are free through a public hospital. After five years from your diagnosis of breast cancer, you can rejoin BreastScreen Aotearoa as long as you are still within the age range of the programme.
Section 4
Breast cancer
Breast cancer in New Zealand
Breast cancer is the most common cancer in New Zealand women. Every year, about 2300 New Zealand women are diagnosed with breast cancer and about 620 die from it. New Zealand has one of the highest breast cancer rates in the world. It is not clear why.
Nearly 10 percent of New Zealand women will develop breast cancer in their lives. Put the other way, over 90 percent of New Zealand women do not get breast cancer. The chances of developing breast cancer are similar for Māori and non-Māori women.
Breast cancer
Breast cancer is a malignant area of the breast. Breast cancer develops slowly over a number of years from the time it starts as a single cell. There are a number of types of breast cancer, and how they develop is not completely understood.
Most cancers start in the milk ducts of the breast (ductal cancers); others start in the lobules of the breast (lobular cancers). When breast cancer spreads into the surrounding breast tissue, it is called invasive breast cancer.
Invasive breast cancer can spread to the lymph nodes, which are the drainage system for the human body. In this way cancer cells can spread to other parts of the body, such as the lungs, bones and liver. Breast cancer can also spread through the bloodstream. Some breast cancers have a better chance of treatment than others.
The risk of being diagnosed with breast cancer increases with age. Breast cancer is uncommon in women under 50. About 70 percent of women who are diagnosed with breast cancer and about 80 percent of women who die from it are 50 years or older.
Some women are at greater risk of breast cancer because there is a history of close family members having the disease. However, most women who develop breast cancer have no relatives with the disease. Even among women who do have relatives with breast cancer, most will never develop it. There is more about family history of breast cancer below.
Ductal carcinoma in situ or DCIS
 Ductal carcinoma in situ is an early form of breast cancer that is contained within the breast duct and has not spread into the surrounding tissue. Although a small number of cases of DCIS are found because there are changes in the nipple or because of a lump, most cases are found through mammography screening. DCIS may show on the mammogram as small specks of calcium in the breast, called microcalcifications. Most microcalcifications are not caused by DCIS.
Ductal carcinoma in situ is an early form of breast cancer that is contained within the breast duct and has not spread into the surrounding tissue. Although a small number of cases of DCIS are found because there are changes in the nipple or because of a lump, most cases are found through mammography screening. DCIS may show on the mammogram as small specks of calcium in the breast, called microcalcifications. Most microcalcifications are not caused by DCIS.
In BreastScreen Aotearoa, about 22 percent of detected cancers are DCIS. DCIS can be low grade, intermediate or high grade. High grade means the cells are multiplying more rapidly, and there is a significantly higher risk the DCIS will progress to invasive cancer. It is not possible to predict which cases of DCIS will develop into invasive cancer.
DCIS is diagnosed in the same way as invasive breast cancer. Treatment is offered to prevent the development of invasive breast cancer. The treatment options depend on the size and grade of the DCIS. If there is a small amount of low-grade DCIS, surgical removal of the area is recommended, usually followed by radiotherapy. If there is a large area, or several areas, a mastectomy may be recommended. For women with small areas of DCIS alone who are not having reconstruction, removal of the lymph nodes is not recommended because of the risk of swelling in the area.
Making a decision about what to do about DCIS is difficult. The area of DCIS may be bigger than what is seen on the mammogram. Not all cases of DCIS develop into invasive cancer, but it is not possible to say which will and which will not. Low-grade DCIS may hide a higher grade DCIS or invasive cancer, or sometimes high-grade DCIS can hide an invasive cancer. Up to one in five women with DCIS diagnosed on a needle biopsy alone will actually have an invasive cancer found at surgery.
If a needle biopsy finds DCIS, surgery is needed to make sure no invasive cancer is present. Some women with low-grade DCIS may choose not to have further treatment after surgery but to wait and see. Studies of women treated in the past for low-grade DCIS with surgical biopsy alone show that in 60 percent of cases the DCIS had not progressed to invasive cancer after 30 years. It is important that all options are discussed with the surgeon and breastcare nurse.
Signs of breast cancer:
- a new lump or thickening
- a change in breast shape or size
- pain in the breast that is unusual
- puckering or dimpling of the skin
- any change in one nipple, such as:
- a turned-in nipple
- a discharge that occurs without squeezing
- a rash or reddening of the skin that appears only on the breast.
These signs may not be caused by cancer. You need to check them with your doctor, even if you have recently had a mammogram.
Breast awareness
Some cancers are found by the woman herself or her partner. You can help find breast cancer early by getting to know your breasts and being aware of any changes that are not normal for you.
Looking at your breasts in the mirror and feeling them while washing or dressing are important as you get older, especially after age 40. This is recommended for all women, even if they are having mammograms. If you notice anything unusual, you should see a doctor to have it checked out.
In the past, some women were taught a formal technique of breast self-examination. This recommendation is no longer made as there is no evidence that this formal self-examination will reduce a woman’s chances of dying from breast cancer. It can also increase a woman’s risk of having unnecessary biopsies.
Examination by a doctor
You can ask your doctor to examine your breasts for you when you visit for another reason. Many doctors, Family Planning clinics and Well Women clinics offer a breast check as part of a cervical smear consultation. About 55–70 percent of breast cancers will be found if a doctor carries out a breast examination. However, there is limited evidence that breast examinations alone, carried out by doctors, reduce the chance of dying from breast cancer.
What causes breast cancer?
Exactly why breast cancer develops in a particular woman is not clear. Breast cancer seems to be linked to hormones, especially the female hormone oestrogen. However, it is unlikely there is one single cause. A combination of factors, some known but others unknown, may trigger or promote the cancer.
Risk factors and protective factors
At present there are no certain ways of preventing breast cancer although there are some clues, known as risk factors and protective factors, about who is more likely or less likely to develop the disease. Many of these risk factors are linked to female hormones, especially oestrogen, for example, age at puberty, age at first pregnancy and age at menopause. Many risk and protective factors are uncertain or controversial.
The risk factors for DCIS appear to be similar to those for invasive breast cancer.
Most studies of risk factors have been done in women of European background, and risk factors may differ for women of different ethnicities.
The risk factors listed on the next page are common amongst women, but there is little they can do about most of them. Some relate to our lives many years before. A few risk factors provide the opportunity to reduce risk by making changes in our lives, but even making those changes cannot give a guarantee.
Women who have the key risk factors should discuss this with their doctors, who can advise them and, if necessary, develop a plan for regular checks that may include mammograms.
Factors that increase the risk of breast cancer
Key risk factors
- Female sex
- Growing older
- Previous breast cancer
- Previous breast biopsy showing a condition that increases risk
- Strong family history – see below
- Inherited genetic factors
- Exposure to repeated or high-dose radiation
Other risk factors
- Ovarian cancer
- Hormone replacement therapy
- Obesity
- Weight gain after 18
- Current drinking of alcohol
- Never had children
- First child after 35
- Oral contraceptives
- Depo-Provera contraceptive injection
- Being a twin
No clear evidence**
- High-fat, red meat diet
- Environmental chemicals, such as pesticides
- Heavy smoking and passive smoking
- Use of statins – medicines to reduce cholesterol
No evidence
- Electric blankets
- Hair colouring
- Abortion or miscarriage
- Tea or coffee
- Underwire bras
- Bruise or injury to the breast
- Personality type
- Stress
- Cellphones, digital clocks, microwaves
- Underarm deodorants
Factors that are protective
Protective factors
- Menstruation starts at late age
- Menopause occurs at a young age
- First child at a young age
- Having children, the more children the greater the protection
- Breastfeeding
No clear evidence**
- Low-fat, high-fibre diet
- Phyto-oestrogens – plant oestrogens
- Exercise
- Green tea
- Regular use of non-steroidal anti-inflammatory drugs
Family history
Women who have a family history of breast cancer may have a greater chance of developing the disease. However, even among women with a family history, most will not develop breast cancer. Only for a very small proportion of women (less than 1 percent) is their family history so significant as to result in a potentially high risk of breast cancer, compared with the general female population. In general, the younger the relative with breast cancer, the more significant the risk. About 4 percent of women will have a moderate increase in their risk of breast cancer by having:
- a mother, sister, daughter or father who developed breast cancer before age 50 or who had cancer in both breasts
- more than one close blood relative on the same side of the family who have had breast or ovarian cancer.
If you are concerned about family history, you can talk to your doctor, who can explain more fully. Your doctor can also refer you to a Regional Genetic Service for assessment.
Section 5
BreastScreen Aotearoa
BreastScreen Aotearoa
BreastScreen Aotearoa, the national breast screening programme, offers free screening mammograms (X-rays) to all New Zealand women aged 45–69 years with no symptoms of breast cancer.
The programme aims to reduce deaths from breast cancer among New Zealand women by detecting cancers when they are small.
BreastScreen Aotearoa organises breast screening services throughout New Zealand. It is part of the National Screening Unit of the Ministry of Health. BreastScreen Aotearoa breast screening services are:
- BreastScreen Waitemata and Northland
- BreastScreen Auckland and North
- BreastScreen Counties Manukau
- BreastScreen Midland (Waikato, Bay of Plenty)
- BreastScreen Coast to Coast (central part of the North Island, including East Coast, Hawke’s Bay, Taranaki, Wanganui, Manawatu and Gisborne)
- BreastScreen Central (Wellington region)
- BreastScreen South (Canterbury, West Coast, Nelson, Marlborough)
- BreastScreen Healthcare (Otago and Southland).
Each BreastScreen Aotearoa service is responsible for ensuring that eligible women in its region are given the chance to enrol in the programme. It must provide services of a high standard and refer women who are found to have cancer to treatment services.
There are also a number of Māori and Pacific health promotion providers.
To contact any of these services, ring freephone 0800 270 200. This automatically connects you to the breast screening service nearest to where you are calling from.
What are the benefits of enrolling with BreastScreen Aotearoa?
- You can receive free mammograms and follow-up assessment if required.
- All your screening mammograms will be kept together and can be used for comparing with future mammograms.
- You will receive two-yearly invitations to have a mammogram.
- If you receive a result that is not normal, you will be followed up.
- The service has quality standards.
- The service is regularly monitored and audited.
- The more women who enrol, the greater the chance the programme will be a success for all New Zealand women.
How can you tell if BreastScreen Aotearoa is working well?
BreastScreen Aotearoa has several ways of checking that the programme is working well.
These include:
- National Policy and Quality Standards set by BreastScreen Aotearoa. These are the standards BreastScreen Aotearoa services are required to comply with. A copy of the standards is available.
- Independent Monitoring Group reports to the National Screening Unit every six months on how well each BreastScreen Aotearoa service is meeting the quality standards. The monitoring reports include recommendations on improvements that can be made. Copies of these reports can be seen on the Health Professional section of the BreastScreen Aotearoa website.
- Regular audits of BreastScreen Aotearoa services to see how well they are meeting the quality standards.
Consumer rights in BreastScreen Aotearoa
Consent to screening
When you contact BreastScreen Aotearoa for the first time, you will be sent a pamphlet about breast screening, along with an appointment time for your first mammogram. If you have questions that have not been answered by the pamphlet, you can discuss these when you attend. Or you can talk it through with your usual health care provider.
If you decide you do want to have regular mammograms with BreastScreen Aotearoa, you will be asked to sign a consent form. This says you consent to having a screening mammogram and you have agreed to enrol in the programme. It also asks you to allow the service to obtain any earlier mammograms you may have had taken elsewhere. It asks you to nominate whether you wish your GP to be informed of the results as well as yourself.
Code of Health and Disability Services Consumers’ Rights
As with all health services, your rights are protected by the Code of Health and Disability Services Consumers’ Rights.
Your rights under the code include:
- a right to receive the information you need to make decisions about your health and about any tests, procedures or treatments and to have the information provided in a way that you understand
- a right to make an informed choice and give your informed consent before you undergo a test, procedure or treatment
- a right to be treated with respect and dignity, taking into account your cultural needs and values
- a right to have a support person with you
- a right to services being provided with reasonable care and skill.
If you want more information about your rights, you can contact the Office of the Health and Disability Commissioner, website www.hdc.org.nz or an independent advocate 0800 555 050 (upper North Island) 0800 423 638 (central and lower North Island) 0800 377 766 (South Island).
How confidential is your information?
BreastScreen Aotearoa must comply with the Health Information Privacy Code. This means it must keep your personal health record and breast X-rays confidential and they must be stored securely.
So that the effectiveness and quality of the programme can be assessed, BreastScreen Aotearoa collects information from public and private providers, the Ministry of Health or its agents, the NZ Health Information Service and the Cancer Registry. The following information about you is collected:
- your name, address, date of birth and National Health Index Number (NHI)
- information about the treatment you have received for your breasts in the past and may require in the future
- relevant medical information
- your mammograms and reports.
As a result of collecting this information, your mammograms will be able to be assessed more accurately, the programme will be able to provide you with any necessary follow-up assessment and you will be invited to attend for your next mammogram.
If you have any questions or concerns about privacy and the confidentiality of your personal health records, you can contact BreastScreen Aotearoa, freephone 0800 270 200, or look at the Privacy Commissioner’s website at www.privacy.org.nz for more information.
How do you make a complaint about any part of the programme?
The Code of Health and Disability Services Consumers’ Rights gives you the right to make a complaint and allows you to make a complaint in a way that is appropriate for you. You should not be treated unfairly in any way because you have made a complaint.
All health services must have a complaints process. You can find out about the complaints process by ringing the particular BreastScreen Aotearoa service you wish to complain about on freephone 0800 270 200.
You can contact an advocate from the Office of the Health and Disability Commissioner to help you with your complaint, freephone 0800 11 22 33.
References
A number of papers were used in the preparation of this booklet. The most significant sources of evidence-based information were the following publications:
Humphrey LL, Helfand M, Chan BKS, Woolf SH. 2002. Breast Cancer Screening: A summary of the evidence for the US Preventive Services Taskforce. Annals of Internal Medicine 137(5): 347–60.
International Agency for Research on Cancer. 2002. Breast Cancer Screening. IARC Handbooks of Cancer Prevention (Vol 7). Lyon: IARC Press.
For further information about the references or the statistics under Benefits and risks of breast screening, contact the National Screening Unit at the Ministry of Health.
Where to go for further information
The inclusion of the websites below does not necessarily demonstrate endorsement of their contents.
New Zealand
National Screening Unit
The National Screening Unit (NSU) is responsible for the BreastScreen Aotearoa Programme. They have a number of publications and a website at www.nsu.govt.nz
There are a number of advisory groups that advise the National Screening Unit on the direction of BreastScreen Aotearoa. These are: BreastScreen Aotearoa Advisory Group, Consumer Reference Group, Māori Advisory Group, and Pacific Advisory Group.
For more about these groups – the names of people on them and how to contact the group – look at the website. The groups can also be contacted through the NSU.
The National Screening Unit contacts are:
PO Box 5013
WELLINGTON
Phone: 04 496 2000
Private Bag 92522,
Wellesley Street,
AUCKLAND
Phone: 09 580 9000
Fax: 09 580 9001
Email: screening@moh.govt.nz
Website: www.nsu.govt.nz
Cancer Society of New Zealand
See phone book for local office.
Cancer helpline: FREEPHONE: 0800 800 426
Email: admin@cancernz.org.nz
Website: www.cancernz.org.nz
Breast Cancer Support Service: Contact your local Cancer Society.
Breast Cancer Network NZ
PO Box 62 666
Kalmia Street
AUCKLAND
Phone: 09 526 8853
Fax: 09 526 8860
Email: brcanz@xtra.co.nz
Website: www.bcn.org.nz
Women’s Health Action
PO Box 9947
Newmarket
AUCKLAND
Phone: 09 520 5295
Fax: 09 520 5731
Email: info@womens-health.org.nz
Website: www.womens-health.org.nz
The NZ Breast Cancer Foundation
PO Box 99 650
Newmarket
AUCKLAND
Phone: 09 523 4397
Fax: 09 523 4396
Toll free line: 0800 902 732
Email: info@nzbcf.org.nz
Website: www.nzbcf.org.nz
International Resources
National Breast Cancer Centre, Australia
Website: www.nbcc.org.au
Breast Cancer Action
55 New Montgomery
Suite 323
San Francisco
CALIFORNIA 94105
Email: info@bcaction.org
Website: www.bcaction.org
Dr Susan Love
SusanLoveMD.org
Post Office Box 846
Pacific Palisades, CA 90272
Fax: 001 310 230 1612
Email: office.administrator@susanlovemd.org
Website: www.dslrf.org/breastcancer
Glossary
Abnormal – not normal, unexpected, unusual.
Anaesthetic – a drug that puts the body to sleep during a medical procedure. If it numbs part of the body, it is called a local anaesthetic; if it puts the whole person to sleep, it is called a general anaesthetic.
Assessment – follow-up tests if something of concern is seen on a mammogram.
Audit – a formal check of a service to see how well it is achieving the standards set for it. Biopsy – removing a sample of tissue from the body and examining it under a microscope to help diagnose a disease.
Biopsy – removing a sample of tissue from the body and examining it under a microscope to help diagnose a disease.
Breast awareness – breast awareness involves a woman knowing what her breasts are like normally, so she can notice any changes that seem different from usual.
Breast cancer – an abnormal growth of cells that is classified as ductal carcinoma in situ or invasive breast cancer.
Breast-conserving surgery – a type of surgery that involves removing a breast cancer, together with a margin of normal tissue. The whole breast is not removed.
Breast implant – a round or teardrop-shaped pouch inserted in the chest to enlarge or restore the shape of the breast. It may be filled with salt water, silicone or another synthetic material.
Breast reconstruction – the surgical recreation of a breast shape after a total mastectomy.
BreastScreen Aotearoa – the national breast screening programme in New Zealand.
Cancer – disease where abnormal cells grow in an uncontrolled way, invading and destroying normal tissue.
Cells – the smallest living unit in the human body. The body is made up of many millions of cells built into tissues and organs.
Chemotherapy – the treatment of disease, especially cancer, with drugs that kill tumour cells.
Clinical – based on history and examination by a doctor or nurse and actual care or treatment of people.
Core biopsy – a needle removes a core of tissue for testing.
Cyst – a closed sac filled with fluid.
Dense breast tissue – made up of less fat and more tightly packed fibrous and glandular tissue, making mammograms harder to read.
Depo-Provera – a hormonal injection to prevent a woman from becoming pregnant.
Diagnose – identifying a disease in a person.
Diagnostic – looking for information to explain an abnormality found on a screening mammogram or ultrasound or on examination.
Discharge – an abnormal trickle of liquid from the nipple.
Duct – a tube for transporting liquid. In the breast, ducts carry milk to the nipple when a woman feeds her baby.
Ductal carcinoma in situ (DCIS) – an area of abnormal cells in the breast duct that has not spread into the surrounding tissue.
Eligible – those women aged from 45–69 who have no symptoms of breast cancer.
Excision – surgical removal of tissue, a tumour or an organ from the body.
False positive – when a woman is told something is not right about her mammogram and further tests show there is nothing wrong.
Fine needle aspiration – a fine needle is put into a breast lump to remove a sample of cells for checking.
General anaesthetic – see anaesthetic.
Hormone replacement therapy (HRT) – hormone treatment for women that eases the symptoms of menopause, or change of life.
Hormone treatment – hormone medications that suppress the growth of hormone-responsive breast cancer.
Independent Monitoring Group – a group of experts outside BreastScreen Aotearoa that checks how well BreastScreen services are achieving the standards set for them.
Interval cancer – cancer diagnosed between regular screening mammograms.
Invasive breast cancer – cancer that has spread into neighbouring normal tissue.
Lobules – sacs in the breast for making milk.
Lymph nodes – glands in the body’s lymphatic system.
Lymphatic system – a network of ducts and glands throughout the body, circulating fluid (lymph) that removes poisonous substances and resists disease. Some cancers can travel to other parts of the body along this system.
Malignant – able to invade normal tissue – cancer.
Mammogram – an X-ray of the soft tissue of the breast.
Mammography – the process of taking a mammogram.
Mammotome – under local anaesthetic, a large needle is inserted in the area of abnormal-looking tissue. Some tissue is then gently vacuumed from the area for testing. This biopsy is often performed with the woman lying on her stomach on a table.
Mastectomy – surgical removal of the breast.
Medical radiation technologist (MRT) (radiographer) – a technician who specialises in taking X-rays.
Menopause (change of life) – the time when a woman’s periods stop and she is no longer able to have children.
Microcalcifications – tiny deposits of calcium in the breast tissue, usually only seen on a mammogram.
Mobile screening units – large mobile clinics that travel around rural and some city areas with the equipment and services needed for screening mammograms.
Multidisciplinary – made up of different specialist areas.
‘No evidence of breast cancer’ – this mammogram result means a woman has a low risk of having breast cancer diagnosed in the next two years.
Non-steroidal anti-inflammatory drugs – a large group of drugs that reduce inflammation (swelling, redness, pain) without using steroids; an example is aspirin.
Obesity – being very overweight. Officially, a person is obese if their weight in kilograms, divided by their height in metres squared (their Body Mass Index), is more than 30.
Oestrogen – a naturally occurring hormone, which in women develops the breasts and is involved in a woman’s menstrual cycle.
Open surgical biopsy – surgery under a local or general anaesthetic, in which a sample of breast tissue is removed for checking by a pathologist.
Oral contraceptives – the contraceptive pill, which contains synthetic hormones and stops women from becoming pregnant.
Organ – a distinct part of the body, for example, lungs, liver.
Outpatient service – a health service that can be visited by people who are not staying in the hospital as patients.
Pathologist – a doctor who studies tissues to check whether they are normal or not.
Protective factors – things that might protect a person from a disease.
Puberty – the time in a girl’s life when she starts having periods and her breasts develop.
Quality standards – targets for measuring the quality of a service.
Radiation – in the case of X-rays, invisible waves sent through the air.
Radiation therapy – the use of high-energy X-ray beams to kill cancer cells or prevent them from reproducing.
Radiographer – (now called a medical radiation technologist) a technician who specialises in taking X-rays.
Radiologist – a doctor who specialises in reading X-ray film.
Radiotherapy – the treatment of disease by radiation.
Reconstruction – the surgical recreation of a breast shape after a total mastectomy.
Risk factors – for breast cancer, things that may make a woman more likely to develop cancer.
Screening – a process in which people who have no symptoms undergo a test or procedure at regular intervals. In some cases (such as mammography), the purpose of screening is to detect cancer at an early stage. In others (such as cervical screening), it is to identify conditions that could develop into cancer.
Screening mammogram – an X-ray of the soft tissue of the breast used as a screening test in women with no signs or symptoms of breast cancer.
Screening programme – an organised effort to screen a population of people to see whether they are likely or unlikely to have a particular condition.
Sentinel node biopsy – a new technique involving the removal of one, two or a few lymph nodes to which breast cancer cells are likely to have spread. This procedure has less pain and fewer complications than removing a number of the lymph nodes in the armpit.
Statins – a class of drugs that reduces the amount of cholesterol made in the body and so reduces the risk of heart attacks and strokes.
Technical repeat film – a repeat mammogram, done because the first one could not be read clearly.
Tissue – a specialised group of cells in the body.
Tumour – an abnormal swelling or lump due to the uncontrolled growth of cells.
Ultrasound – a test using sound waves to produce a picture of tissues inside the body.
Vacuum-assisted biopsy – vacuum suction is used to assist the removal of a sample of tissue through a needle.
X-ray – invisible waves of radiation passed through the body onto a photographic plate to enable diagnosis of abnormal tissue.
Index
scarring following ..... 25
types of ..... 31–33, 37, 42
core ..... 31, 32
fine needle ..... 31, 32
Mammotome ..... 31, 32
needle ..... 31, 32, 41
open surgical ..... 32, 33, 41
sentinel node ..... 37
vacuum-assisted ..... 31, 32
wire localisation open ..... 33
breast
see also breast cancer
dense tissue ..... 9, 20
description of normal ..... 9
fatty tissue ..... 9, 20
lobules and ducts ..... 9, 40
breast awareness ..... 42
see also ductal carcinoma in situ (DCIS)
and age ..... 40
causes of ..... 43
definition of ..... 40
diagnosis of ..... 31–33
see also ultrasound
see also biopsies
family history ..... 40, 45
in New Zealand ..... 40
invasive ..... 40, 41
lymph nodes ..... 37, 40
protective factors ..... 43, 44
reconstruction after ..... 37
risk factors ..... 43, 44
support for ..... 35, 54–55
symptoms of ..... 15, 42
treatment for ..... 35–38
chemotherapy ..... 37
mastectomy ..... 36, 37, 41
radiotherapy ..... 35, 36, 41
removal of lymph nodes ..... 37
sentinel node biopsy ..... 37
surgical removal of lump ..... 36
types of ..... 40
breastcare nurse ..... 14, 29, 30, 35, 36, 37
breast examination by a doctor ..... 42
breast implants ..... 16
breast self-examination ..... 42
see also consumer rights
see also quality standards
aims of ..... 48
age range ..... 10, 16, 48
audits ..... 49
benefits of ..... 49
complaints about ..... 52
consent to ..... 16, 50
cost of ..... 14
eligibility for ..... 10, 15
enrolment in ..... 10, 50
locations ..... 10–11, 48
mobile screening units ..... 11, 15
monitoring ..... 49
privacy ..... 51, 52
quality standards in ..... 49
women 70 or over ..... 16
women who have had breast cancer ..... 15, 38
women with a disability ..... 15
breast screening ..... 8–16
see also mammograms
see also BreastScreen Aotearoa
aim of ..... 8
benefits and risks for: ..... 18–25
women over 50 ..... 18–19
women under 50 ..... 20–22
cancer ..... see breast cancer
consent ..... see informed consent
consumer rights ..... 50–52
ductal carcinoma in situ (DCIS) ..... 25, 35, 41
grades of ..... 41
risk factors for ..... 43
treatment of ..... 41
Health and Disability Commissioner ..... 50–52
advocates ..... 51
Code of Rights ..... 50–52
informed consent ..... 16, 33, 50
abnormal ..... 12, 29, 31
accuracy of ..... 9, 20, 22–24
and breast implants ..... 16
and dense tissue ..... 9
and large breasts ..... 13, 25
and small breasts ..... 13
and symptoms of breast cancer ..... 15
assessment of abnormal results ..... 29, 30, 31, 34, 35
definition of ..... 8, 23
how performed ..... 12
limitations and risks of
false positives ..... 20, 22, 23
interval cancers ..... 24
missed cancers ..... 24
over-diagnosis and over-treatment ..... 22, 23, 25
radiation risk ..... 20, 22, 25
pain during ..... 13
preparing for ..... 11
privacy during ..... 11, 30, 51
results of ..... 28–29
support during ..... 14, 30, 50
technical repeat mammograms ..... 14
mammography screening ..... see breast screening
medical radiation technologist (MRT) ..... 12, 13, 30
microcalcifications ..... 41
multidisciplinary team ..... 30, 35
National Screening Unit ..... 53–54
oestrogen ..... 43
support
during mammograms ..... 14, 30, 50
for breast cancer ..... 35
treatment for breast cancer ..... see breast cancer
Acknowledgement
This booklet was prepared by Women’s Health Action (WHA) Trust for BreastScreen Aotearoa. WHA would like to thank all those involved in the preparation of this booklet. Special thanks to the women who attended focus groups and the women who agreed to have their photographs included in the booklet. Thanks also to those working in the health sector, women’s organisations and others who made comments on various drafts of this booklet during its development.
Tēnā koutou katoa.
Remember:
Women of any age who feel or notice anything unusual about their breasts, at any time, should see their doctor.
0800 270 200
www.nsu.govt.nz
Published 2007 for the Ministry of Health by Learning Media Limited, Box 3293, Wellington, New Zealand.
Copyright © Ministry of Health 2007
ISBN 978-0-478-29924-3 (print)
ISBN 978-0-478-19125-7 (online)
* Details of who is eligible for publicly funded (free or subsidised) personal health and disability services in New Zealand can be seen at www.health.govt.nz/eligibility
** No clear evidence means that the results of studies have been mixed, or there is not enough evidence to say that it is proven.