Sleep on side when baby's inside - HE2551
Gives clinical information to inform health professionals about how advising people to sleep on their side in the 3rd trimester of pregnancy is proven to reduce the risk of stillbirth by half.
The full resource:
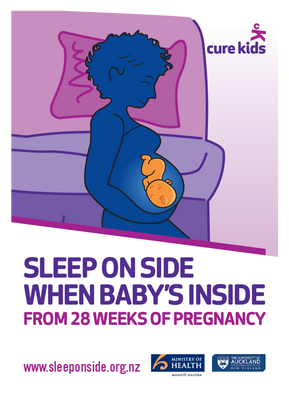
Sleep on side when baby's inside from 28 weeks of pregnancy
Information for Health Professionals: Maternal Supine Going to Sleep Position and Late Stillbirth Risk
Key messages for health professionals to discuss with all pregnant women:
- Going to sleep on your side (either left or right side) from 28 weeks of pregnancy halves your risk of stillbirth compared with going to sleep on your back
- The important thing is to start every sleep (daytime naps and going to sleep at night) lying on your side and settle back to sleep on your side if you wake up
Epidemiology
Late stillbirth (≥28 weeks’) occurring in singleton non-anomalous pregnancies affects approximately three in every 1000 women, resulting in deaths of approximately 160 New Zealand babies annually. Identification of modifiable risk factors has the potential to reduce this tragic pregnancy complication.
Four published studies from New Zealand (n=2), Australia (n=1) and the United Kingdom (n=1) have now reported that women who go to sleep lying on their backs in the third trimester of pregnancy have an increased risk of stillbirth, that is independent of other stillbirth risk factors.1-4 This consistent finding is biologically plausible (see below) and is important as going-to sleep position is a modifiable risk factor for late stillbirth.
Physiology
When a healthy mother lies on her back (supine position) in late pregnancy the uterus compresses the main abdominal vein [inferior vena cava (IVC)] reducing the IVC blood flow by >80%. The aorta is also partially compressed by the pregnant uterus with an approximate 30% reduction in flow.
The mother’s circulatory system compensates for this reduction in IVC flow when lying on her back by increasing blood flow back to the heart through collateral veins below the obstruction and increasing her heart rate.5 However, this does not fully maintain optimum blood flow.
The physiological response to the supine maternal position in late pregnancy includes:
- Reduction in venous return to the heart by approximately 24%
- Reduced cardiac output on average by 16% which is likely to reduce uterine and placental blood flow leading to reduced oxygen delivery to the fetus
The fetal response
When healthy pregnant women lie on their back in the third trimester the fetus responds by spending more time in a quiet behavioural state (non-reactive fetal heart pattern) and rarely exhibits a very active behavioural state. This suggests that the healthy fetus responds acutely to the reduced blood flow by conserving oxygen consumption.6
We speculate that whilst the healthy fetus can compensate adequately for periods of reduced placental perfusion an at risk or vulnerable fetus is likely to become acidotic and decompensate.
Sleep-disordered breathing
Sleep-disordered breathing increases in pregnancy, can be associated with maternal hypoxic episodes and is more common when lying on the back. Sleep-disordered breathing has been associated with pregnancy complications including fetal growth restriction, hypertensive disorders and gestational diabetes which are all associated with increased stillbirth risk.7 Sleep-disordered breathing while lying on the back could therefore add to the adverse effects of reduced blood flow.
References
- Stacey T, Thompson J, Mitchell EA, Ekeroma AJ, Zuccollo JM, McCowan LM. Association between maternal sleep practices and risk of late stillbirth: a case-control study. BMJ 2011; 342:d3403.
- McCowan L, Thompson J, Cronin R, et al. Going to sleep in the supine position is a modifiable risk factor for late pregnancy stillbirth; Findings from the New Zealand multicentre stillbirth case-control study. PLOS One 2017; 12(6): e0179396.
- Gordon A, Raynes-Greenow C, Bond D, Morris J, Rawlinson W, Jeffery H. Sleep position, fetal growth restriction, and late-pregnancy stillbirth: the Sydney stillbirth study. Obstet Gynecol 2015; 125(2):347-55.
- Heazell A, Li M, Budd J, Thompson J, Stacey T, Cronin RS, Martin B, Roberts D, Mitchell EA, McCowan L. Association between maternal sleep practices and late stillbirth – findings from a stillbirth case-control study. BJOG 2018 125(2):254-262.
- Humphries A, Ali Mirjalili S, Tarr GP, Thompson JMD, Stone P. The effect of supine positioning on maternal hemodynamics during late pregnancy. J Matern Fetal Neonatal Med 2018; Epub 17 May 2018: doi.org/10.1080/14767058.2018.1478958.
- Stone PR, Burgess W, McIntyre JP, Gunn AJ, Lear CA, Bennet L, Mitchell EA, Thompson JM. Effect of maternal position on fetal behavioural state and heart rate variability in healthy late gestation pregnancy. J Physiology 2017; 595(4):1213-1221.
- O’Brien LM. Sleep-Disordered Breathing in Pregnancy. Current Sleep Medicine Reports 2016; 2(4): 183-190.
