Well Child Tamariki Ora My Health Book - HE7012
Parent information and health and immunisation record for babies and children, 0–5 years. Includes information on child safety and illness.
If you need a copy for personal use, please contact your health provider. We do not usually send books to individuals.
Find out more at Te hapūtanga me ngā tamariki | Pregnancy and children and Well Child Tamariki Ora providers
The full resource:
Contents
How to use this book
All about your child
Well Child Tamariki Ora assessments
Learning and growing
Looking after yourself
Partners are needed too
Keeping your child healthy and safe
Emergencies – urgent action needed
Contacts and information
Danger signs
How to use this book
Welcome, Kia ora koutou katoa, Tālofa lava, Kia orāna, Fakalofa lahi atu, Tāloha ni, Ni sa bula vinaka, Tālofa koutou, Mālō e lelei.
This book belongs to you and your child. The words ‘you’ and ‘your’ mean anyone who will love and care for this child – parent, partner, foster parent, grandparent, whānau, family, babysitter or childcare worker.
In it, you will find information as well as places to record your child’s development in the first 5 years.
Keep it somewhere safe, and use it to write down all the special and important things that happen to your child.
When your child sees a doctor, nurse or other health professional, they will need to record your child’s health and development information. Please take this book with you every time you take your child to a health appointment or hospital visit.
If the meaning of any page in this book is not clear, ask your Lead Maternity Carer, nurse or doctor to explain it.
Mehemea kāore ngā kōrero o tēnei pukapuka e marama ana, me pātai atu ki tētahi nēhi kia whakamāramatia.
Afai e i ai se faamatalaga o i so‘o se itulau o lenei tusi e te le malamalama atoatoa i ai, ia fesili i se tasi, e pei o le tama‘ita‘i tausima‘i, o le a mafai ona ia faamaninoina.
Me kare te aiteanga ki roto i teia puka e marama ana, e ui atu ki tetai tangata mei te neti, kia akamarama mai.
Kaeke kua fai he tau lau he tohi nei kua nakai maama e koe, ti hūhū atu ke he ha tagata tuga e nosi ke fakamaama atu e ia kia koe.
Kapau ‘oku ta‘e mahino ha me‘a ‘i he tohi ni, ‘eke ki ha taha hange ko ha Neesi.
Kafai he fakamalamalamaga i tenei tuhi e he manino, fehili ki he tino ve ko te teine tauhi tauale ke fakamatala atili atu.
All about your child
Well Child Tamariki Ora programme
Disability and Well Child Tamariki Ora
Immunisation
The Community Oral Health Service
Recording your child’s development
Growth charts for all children
Well Child Tamariki Ora programme
You and your child have the right to use the free Well Child Tamariki Ora service. The three parts of the service will support you to ensure your child grows and develops to their full potential:
-
Health and development assessments
Providing reassurance that your child is developing as expected, through growth and development assessments; and informing you about other services to keep your child healthy. -
Care and support for families and whānau
Supporting and helping you and your family/whānau to identify your needs as you care for your child, and linking you with community and other services.
-
Health education
Supporting you to gain the knowledge and skills to respond to your child’s needs at the different stages of their development.
EAC are provided to tamariki/children and their whānau/families who are at risk, first-time parents and have high needs.
This care is provided by Well Child Tamariki Ora Providers when identified by the LMC or local Primary Maternity Team.
When: Before birth
Lead Maternity Carer
A Lead Maternity Carer is usually a midwife, but may also be an obstetrician or a general practitioner with additional training in caring for pregnant women and babies.
When: Birth, 24 to 48 hours, First week
Transition of care from Lead Maternity Carer to Well Child Tamariki Ora provider
During these weeks your care moves from the Lead Maternity Carer to a Well Child Tamariki Ora provider. Your Lead Maternity Carer provides you with a choice of Well Child Tamariki Ora providers in your area.
When:
Lead Maternity Carer: 2 to 6 weeks
Well Child provider: 4 to 6 weeks
General practitioner
This assessment includes the 6-week immunisations, hip screening and vision check (including red reflex as for the birth assessment).
When: 6 weeks
Well Child Tamariki Ora provider
A Well Child Tamariki Ora provider is usually a nurse who has additional training in supporting parents/caregivers to care for their babies and preschool children. The nurse may be employed by a range of organisations including Plunket, a Māori Well Child Tamariki Ora provider, a Pacific Well Child Tamariki Ora provider, a general practice team, or a public health service.
There may also be times when you and your baby will be seen by a general practitioner for a Well Child assessment.
When: 8 to 10 weeks, 3 to 4 months, 5 to 7 months, 9 to 12 months, 15 to 18 months, 2 to 3 years, B4 School Check
For the schedule of immunisations, see the Immunisation section.
Health appointments
Well Child Tamariki Ora health assessments are timed to match with important stages in your child’s life. More visits may be arranged if you and your child need additional care and support.
See the 24–48 hours assessment
Additional Antenatal Contacts
See the 2–6 weeks LMC final assessment
Lead Maternity Carer completes referral forms to Well Child Tamariki Ora provider and general practitioner
6 weeks: Immunisation, hip screening, vision check
See the 9–12 months assessment
See the 15–18 months assessment
Vision and hearing screening
Vision and hearing screening, part of the Well Child Tamariki Ora service, is designed to identify hearing problems at birth and specific vision and hearing problems at around 4 to 5 years and at 11 years. Your child will be offered hearing screening soon after birth, and vision and hearing screening as part of their B4 School Check and then at school when they are 11.
Disability and Well Child Tamariki Ora
Nau mai, haere mai! This part is for disabled parents and/or whānau who have a baby with an impairment, health condition or disability.
In New Zealand, 1 in 6 people has a disability. For children, it’s about 1 in 10. Disabled New Zealanders are in all our communities. The Well Child Tamariki Ora programme is here to help all children and their families - including those with impairments, health conditions or disability.
Meeting your disability needs
Everyone experiences disability differently. What one whānau might need could be very different from what another whānau might need. If there’s something that would make things easier for you, tell your healthcare provider.
You might need things like: accessible parking close to the entrance, New Zealand Sign Language interpreters for appointments, flexible appointment times to fit in with your schedule, accessible information or alternative formats, having a support person with you, quiet spaces.
It might feel hard to talk about, but it’s important to tell your healthcare provider about your disability needs so they understand how best they can meet your needs.
If your pēpi has an impairment, health condition or disability
Congratulations on your new pēpi! Try to connect with people and groups who might understand what’s happening for you. There are many different community groups (either by disability type or where you live) where many parents share advice and support. Community groups can be found on social media sites and at Disability Services — Pēpe Ora
You might need to start using different types of health and disability services. As part of this, you may be getting new information and have to make different choices. You can ask your healthcare provider if there is someone (like a kaiāwhina) who can help you. Disability community groups and organisations have a lot of helpful information.
And remember - take time to enjoy your new pēpi, dream big and have high hopes. Celebrate the wonderful things they do no matter how big or small.
Where to find help
Firstport is a great place to start looking at the range of supports and services that can help your whānau Disability information and support services | Firstport
Immunisation
Immunisation is your child’s best protection
Immunisation saves lives. Getting your tamariki (children) immunised is one of the best ways to protect them and set them up for a healthy future. The World Health Organization, Health New Zealand | Te Whatu Ora, the New Zealand Ministry of Health and medical authorities all recommend that children be fully immunised.
Immunisation teaches your child's body how to fight off infectious diseases and reduces the risk of potentially life-threatening illness.
Immunising your child also protects other vulnerable people in your whānau and community who might not be able to get vaccinated themselves.
When to immunise
Your child's immunisation journey starts before birth. When you're pregnant, it's recommended, and free, to be immunised against diseases like flu and whooping cough which can harm you and your pēpi (baby). This will also provide pēpi with some protection when they are born until they are old enough to be immunised themselves.
Once your baby is born, they can get regular immunisations against a range of preventable diseases, including whooping cough, chickenpox and measles.
These immunisations are given at specific times throughout your child's life to provide them with the best possible protection. Recommended vaccines for all tamariki are on the National Immunisation Schedule. This is like a timetable that shows when each vaccine is due.
The immunisations protect against:
- diphtheria
- haemophilus influenzae type b (Hib)
- hepatitis B (hep B)
- human papillomavirus (HPV)
- measles
- meningococcal B
- mumps
- pertussis (whooping cough)
- pneumococcal disease
- polio
- rotavirus (gastroenteritis)
- rubella (German measles)
- tetanus
- varicella (chickenpox).
The National Immunisation Schedule
6-week immunisations
- Rotavirus (dose 1 of 2)
- Diphtheria, tetanus, whooping cough, polio, hep B, and Hib (dose 1 of 3)
- Pneumococcal (dose 1 of 3)
3-month immunisations
- Rotavirus (dose 2 of 2)
- Diphtheria, tetanus, whooping cough, polio, hep B, and Hib (dose 2 of 3)
- Meningococcal B (dose 1 of 3)
5-month immunisations
- Diphtheria, tetanus, whooping cough, polio, hep B, and Hib (dose 3 of 3)
- Pneumococcal (dose 2 of 3)
- Meningococcal B (dose 2 of 3)
12-month immunisations
- Measles, mumps, and rubella (dose 1 of 2)
- Pneumococcal (dose 3 of 3)
- Meningococcal B (dose 3 of 3)
15-month immunisations
- Hib (booster)
- Measles, mumps, and rubella (dose 2 of 2)
- Chickenpox (single dose)
4-year immunisations
- Diphtheria, tetanus, whooping cough, and polio (booster)
From age 9
- HPV (2 doses, 6 months apart)
From age 11
- Tetanus, diphtheria, whooping cough (booster)
For more information visit Immunisations
For the best protection, your pēpi need all their immunisations
It's important your child has all their immunisations, at the recommended times. Not getting them immunised on time will put your tamariki at greater risk of getting a serious disease.
You can create a personalised immunisation schedule for your tamariki that shows what immunisations they need and when they're due at Create a child’s personalised immunisation schedule If you're not sure if your tamaiti has been immunised, is overdue, or eligible, talk to their doctor, nurse or Well Child Tamariki Ora provider.
If your child has missed an immunisation, it's OK. Tamariki can catch up on most vaccinations.
Where to get your tamariki immunised
To book an immunisation appointment, contact your child's doctor, nurse, or Well Child Tamariki Ora provider. Immunisations are also available through some pharmacies, school programmes, Māori and Pacific health providers, and community vaccination events. Many immunisations including flu, measles and pregnancy vaccines can be booked online at BookMyVaccine.nz
You can call the Vaccination Helpline 0800 28 29 26 to ask questions or for support to book appointments for your child, yourself or your whānau. They are available from 8.30am to 5pm, Monday to Friday (except public holidays). Interpreters are available and you can choose to speak with a Māori advisor, a disability advisor or use New Zealand Relay Services
Additional vaccines
Extra vaccines may be recommended if your child is considered 'high-risk,' for example they have a health condition or they are travelling overseas. These vaccines may include tuberculosis (TB) immunisation for those children who have family members with TB or who will be staying for longer than 3 months in a country which has a high TB rate.
Ask your doctor, nurse, or Well Child Tamariki Ora provider what additional immunisations your tamariki may need.
All vaccines in New Zealand have been thoroughly assessed for safety and effectiveness.
What happens during the appointment
Your vaccinator will talk to you about your child's immunisation and what to expect afterwards. There will be time to ask questions and you will be asked if you're happy to go ahead with the immunisation. In some situations you might need to sign a consent form.
Let the vaccinator know if you or your child are scared of needles. They're trained to make you as comfortable as possible. They can provide distractions and techniques to help reduce pain and anxiety. You need to allow at least 30 to 45 minutes for the whole vaccination appointment. This includes waiting time after the vaccination.
Tips for pēpi and tamariki immunisations
- Talking, cuddling, and holding your tamariki will help distract them from the injection and soothe them afterwards if they’re upset.
- Try to stay calm. Babies and children can tell when their parents are feeling anxious.
- Feeding your baby (including breast or bottle feeding) while they’re being immunised may help them feel more comfortable.
What to bring
- Bring your child's Well Child Tamariki Ora My Health book along to the appointment so the vaccinator can update the immunisation history. Don’t worry if you do not have the book, immunisations are also recorded in the Aotearoa Immunisation Register.
- Choose clothes that can be removed or rolled up so the vaccinator can access the upper arm or thigh. Babies under 12 months have all their injections in their thigh. From 1 year, tamariki have their injections in the arm or thigh.
- Bring any food/kai or drink you’ll need during this time.
- You can bring your child’s favourite toy, blanket, game, or book along as a distraction and to keep them busy afterwards.
- If you’re nervous, bring a whānau member or friend for support.
- You do not need to bring ID to the appointment.
After your child's immunisation
You'll be asked to wait up to 20 minutes after the vaccination to make sure your tamaiti and you are feeling OK.
Possible side effects and reactions
Some people experience mild reactions after immunisation. They may develop a fever or experience tenderness, swelling and redness where the injection was given. This is the body’s normal response to immunisation and shows the vaccine is working. Symptoms usually settle after a day or two. If you do not experience any side effects that’s OK too, the vaccine is still working.
Refer to Fevers – what to do
Allergic reactions
Serious allergic reactions are extremely rare. Only about 1 in 1 million people will experience this.
Your vaccinator is well-trained, knows what to look for and can treat an allergic reaction quickly if it happens.
Serious allergic reactions normally happen quickly after vaccination. This is why you need to wait for up to 20 minutes after immunisation.
Every vaccine can cause different reactions
At the appointment, your vaccinator will let you know what reactions to look out for. You will be told what to expect, how to manage any reactions and when to seek help.
For example, some pēpi, tamariki or adults may develop a fever or a mild rash. This is an expected response after some vaccines, and usually does not last long. It does not mean your child is sick.
How to treat common reactions in children
Some ways you can make your child more comfortable after their vaccination include:
- If their arm or leg is sore from the injection, put a wet cloth or ice pack (wrapped in a dry cloth) on it. Do not rub the injection site.
- If they have a fever, keep your child hydrated. Provide them with lots of water to drink. If breastfeeding, give your child lots of feeds.
- If your child gets too hot, reduce the amount of clothing they are wearing.
- Give your child lots of cuddles.
Give paracetamol or ibuprofen as advised by your doctor, nurse, or Well Child Tamariki Ora provider.
If you are concerned about your child after a vaccine, contact your doctor or nurse or call Healthline (0800 611 116 at any time).
See also the Danger Signs for Baby and Child Sickness
Serious reactions are rare, but can include:
- wheezing, shortness of breath or difficulty breathing
- pinkish, itchy swellings on the skin, also called hives or nettle rash
- swelling of the face, lips, tongue which may cause difficulty in swallowing or breathing, or
- swelling of other parts of the body.
If your child is having a serious reaction, call 111 and make sure you tell the call handler that a vaccine was given.
Immunisations given overseas
Some people living in Aotearoa may have received all or some of their childhood immunisations overseas. They should ask their nurse or vaccinator to check their overseas immunisation records to ensure they are fully protected in New Zealand
and to ensure these are added to the Aotearoa Immunisation Register.
Additional vaccines may be recommended and the vaccinator will be able to schedule these. They will also be able to update New Zealand immunisation records to show any doses given in other countries. If you don’t have copies of overseas records re-vaccination may be recommended.
Vaccine-preventable diseases on the National Immunisation Schedule
Diphtheria
Diphtheria is a serious disease that can easily spread from person to person (especially within families) through coughing and sneezing.
It causes a skin infection but can also affect the throat causing breathing difficulties. Diphtheria was a common cause of death in children until the 1940s, but this disease is now very rare in New Zealand because of immunisation.
Hepatitis B (hep B)
Hepatitis B can easily spread through contact with the blood or bodily fluids (like saliva) of an infected person. For example, it can spread through cuts and scratches, or by sharing a drink bottle with an infected person.
It’s a viral infection that can cause serious problems, including liver disease and liver cancer. Hepatitis B cannot be cured but can be prevented with vaccination.
Hepatitis B was a common disease in New Zealand until a vaccine was introduced in the 1980s.
Haemophilus influenzae type b (Hib)
Hib is a bacteria that causes life-threatening illnesses in young children. It’s spread through the air by breathing, coughing and sneezing.
It most often leads to:
- meningitis – an infection of the membranes that cover the brain and spinal cord
- epiglottitis – an infection and swelling in the throat that makes it difficult to breathe.
Although doctors can treat Hib with antibiotics, some children still die. Others risk permanent brain and spinal cord damage.
Measles
Of all diseases, measles is one of the most dangerous and contagious. It’s so infectious that, if you’re not vaccinated and come into contact with someone who has measles, you’re very likely to catch it and pass it on to others.
Measles spreads through coughing and sneezing. It can cause a rash, ear infection, diarrhoea, and seizures caused by fever. Measles can also lead to pneumonia, which is the main cause of death from measles.
Meningococcal B
The meningococcal B vaccine was added to the National Immunisation Schedule for babies on 1 March 2023. All tamariki under 5 years old can catch up for free.
Meningococcal disease is an infection caused by bacteria.
It can lead to two very serious illnesses:
- meningitis – an infection of the membranes that cover the brain and spinal cord
- septicaemia – blood poisoning.
There are different types of meningococcal bacteria, including A, B, C, W, and Y. In New Zealand, most meningococcal disease is caused by group B bacteria.
Mumps
Mumps is an infectious illness caused by a virus. It leads to painful swelling in the salivary glands around the face.
In rare cases, there can be serious complications such as:
- hearing loss
- meningitis – an infection of the membranes that cover the brain and spinal cord
- encephalitis – inflammation of the brain.
Mumps can cause swelling of the testicles or ovaries if a person is infected after puberty. Effects on fertility are extremely rare in males and unconfirmed in females.
Pertussis (whooping cough)
Whooping cough (pertussis) is a bacteria that causes breathing difficulties and severe coughing fits. The cough can go on for weeks or months which is why it’s sometimes called the ‘100 day cough’.
Having severe whooping cough can lead to pneumonia, seizures, and other neurological (brain) issues. More than half of babies under 12 months old who catch it need to go to hospital, and up to 1 in 50 of these babies dies.
It’s very contagious. It can easily spread between family members by coughing and sneezing. It can also spread quickly around early childhood centres and schools.
Pneumococcal disease
Pneumococcal disease is caused by bacteria that live in your throat. These bacteria do not normally cause problems, but if they spread to other parts of the body they can make you very sick. Pneumococcal disease is easily spread by coughing, sneezing, and close contact. Pneumococcal bacteria can cause minor infections, like:
- sinusitis – infection of the sinuses
- ear infections.
Pneumococcal disease can also lead to life-threatening conditions, like:
- pneumonia
- meningitis – an infection of the membranes that cover the brain and spinal cord
- septicaemia – blood poisoning.
Polio
Polio is a highly contagious disease caused by a virus.
Symptoms include headache, diarrhoea, tiredness, and pain in the limbs, back and neck.
In serious cases, it can cause paralysis (muscle weakness) and death. About 1 in 20 hospitalised patients dies and up to 1 in 50 patients who survives is permanently paralysed. There is no cure for polio – it can only be prevented by immunisation.
Rotavirus (gastroenteritis)
Rotavirus is a viral infection that causes diarrhoea, vomiting and fever. It most often affects babies and young children. Some tamariki get so sick they need to go to hospital.
Immunisation against rotavirus will protect around 8 out of 10 babies from severe rotavirus infection. Almost all children who are not immunised get a rotavirus infection before they are 5 years old.
Rubella (German measles)
For children, rubella is usually a mild viral illness that causes a spotty rash. If you catch it when you are pregnant, however, it can cause serious birth defects in your baby (such as deafness, heart defects, and brain damage).
Tetanus
This rare but serious disease is caused by bacteria found in soil and manure (horse or cow poo). You can get the disease if dirt carrying this bacteria gets into a wound – for example, if your tamariki get a cut while playing in the garden.
Varicella (chickenpox)
Infections are normally mild, but chickenpox can make some people very sick. It’s usually more severe in rangatahi (young people) and adults and for people with a weakened immune system.
Travelling overseas with children
It’s important to ensure everyone in the family is up to date with their immunisations before travelling.
There may be additional vaccines recommended by your doctor (these may need to be paid for) and some of the regular vaccines may be offered early if travelling to a country with an outbreak of disease. One of the most important vaccines to make sure everyone has had before travelling is the measles vaccine - babies under 12 months of age may be recommended to receive an extra early dose of their MMR vaccine, which is called dose zero. They will still need their MMR dose one at 12 months and MMR dose two at 15 months.
Visit Immunisations to learn more about these vaccines and diseases
Aotearoa Immunisation Register (AIR)
Your child‘s immunisations will be recorded on the Aotearoa Immunisation Register (AIR).
The AIR helps authorised health professionals find out what vaccines a child has been given, and what they are due to get. This helps understand risk to your child if they are exposed to a vaccine-preventable disease. It will also provide valuable information about the population’s protection against disease. Ask your health professional if you want to know more about the AIR, or visit tewhatuora.govt.nz/air
You can request to restrict access to the immunisation history for children in your care (aged 16 years and under), or other dependents, if you have legal authority to do so. Refer to the AIR webpages for further guidance and important things to consider.
Aotearoa Immunisation Register (AIR) – Health New Zealand | Te Whatu Ora
AIR privacy information – Health New Zealand | Te Whatu Ora
Immunisation record (to be completed by your vaccinator)
Immunisation certificate (to be completed by your vaccinator)
My Health Record
Getting enrolled with a general practice (GP)
It’s free to enrol with a general practice – and many services for tamariki aged under 14 are free, including immunisation.
General practices normally charge a higher fee, often called a casual rate, for patients that aren’t enrolled with their practice.
For more information about enrolling with a GP visit Healthpoint or call Healthline on 0800 611 116
Next steps in your child’s immunisation journey
- Talk to your Lead Maternity Carer, doctor, nurse or Well Child Tamariki Ora provider
- Health New Zealand | Te Whatu Ora: Immunisations
- Healthline can also support whānau to access vaccinations if they don’t have a GP or can’t get an appointment. Freephone Healthline 0800 611 116
- Call the Vaccination Helpline 0800 28 29 26 to book or ask vaccination questions over the phone from 8.30am to 5pm, Monday to Friday (except public holidays). Interpreters are available and you can choose to speak with a Māori advisor,
a disability advisor, or use New Zealand Relay Services They can also support whānau to access immunisations if they don’t have a GP or can’t get an appointment.
The Community Oral Health Service
Healthy teeth right from the start
Healthy teeth play an important role in a child’s development. Baby teeth are very important for chewing and proper speech development. They also save the space for adult teeth and are important for the proper growth of the face and jaw. Baby teeth need to be looked after and valued.
Children’s teeth are at risk of tooth decay as soon as they begin to break through the gum, usually around the age of 6 months. Tooth decay is largely preventable by brushing the teeth with fluoride toothpaste, eating a healthy diet that is low in sugar, and having regular dental check-ups from an early age. There is advice throughout this book on caring for your child’s teeth, including teething, toothbrushing with fluoride toothpaste and a healthy diet that is tooth-friendly.
Free oral health care
Children in New Zealand are entitled to free basic oral health services from birth until their 18th birthday. Enrol your child at birth with your local Community Oral Health Service. The service is free and supports parents/caregivers and family/whānau to actively participate in their child’s oral health care and to care for their child’s teeth at home.
The oral health service focuses on preventing dental problems and recognising and treating any problems as early as possible. Regular dental visits are vital from an early age.
It’s easy to enrol your child in the oral health service, just call 0800 TALK TEETH, 0800 825 583. Staff will guide you through how to enrol and will send out the right forms for you to fill in.
It is important to enrol your child as early as possible so that you can arrange the first dental check-up.
Your dental or oral health therapist will let you know how often you need to take your child. Regular check-ups mean that problems with your child’s teeth can be picked up early.
The first visits to the dental or oral health therapist will be an unfamiliar experience for your child. You can help make it easier for them by getting an appointment for a time when they are not likely to be tired and by being positive about dental visits. Use positive language with your child, such as ‘keeping your teeth healthy’ and ‘keeping your smile beautiful’.
Your Well Child Tamariki Ora provider or doctor can also give advice to help you keep your child’s teeth healthy or make referrals to specialist care if needed.
If you wish, you can choose to seek dental care for your child from private dental practitioners, but this will be at your own cost.
Baby teeth
The lower front teeth usually come first. These are followed by the upper front teeth. As each tooth comes, you can write your baby’s age on that tooth in the picture (shown below, and on page 32 of your Well Child Tamariki Ora My Health Book).
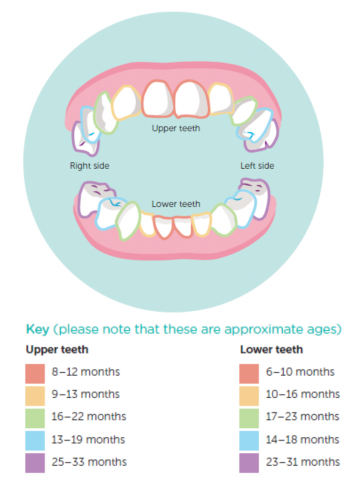
For more information on teething and caring for teeth, see Teething (age 6 weeks to 6 months), Looking after baby teeth (age 6 months to 12 months), Teeth – time to teach brushing twice a day (age 1 and 2 years), Caring for teeth (age 2 to 3 years), Preschoolers’ teeth (age 3 to 5 years) and Looking after your child’s teeth.
Recording your child’s development
The following pages are for you and your Well Child Tamariki Ora providers to record and follow your child’s development.
For information on how children develop at different ages, see the appropriate part of the Learning and growing section.
Growth charts for all children
Growth is an important measure of children’s health and wellbeing. The following ten growth charts are suitable for use with New Zealand children up to 5 years of age. They are based on measurements collected by the World Health Organization in six different countries and their format is adapted from growth charts used in the United Kingdom.
Because children grow at varying rates at different ages, we can only understand whether a measurement is normal by comparing it with the normal range of measurements for other children of the same age and gender. Growth charts use these measurements to show the range within which most healthy children are expected to grow and the growth patterns of an individual child over time.
These growth charts use nine centiles, shown as lines drawn in curved patterns. Each line at a particular centile marks the weight or height below which that percentage of children of that age and gender fall. For example, 25 percent of children are lighter than the 25th centile for weight, or shorter than the 25th centile for height. The 50th centile represents the median (middle) of the population.
Healthy children grow along or next to any of the centile lines. What matters is that their growth curve stays steady, with no sudden jump or drop.
For more information see the Ministry of Health’s Fact Sheet 1: What Are Growth Charts and Why Do We Need Them?
The following ten growth charts were originally based on UK-WHO growth charts and used the UK-WHO combined data set developed by the Royal College of Paediatrics and Child Health, United Kingdom. For information about Body Mass Index (BMI) and healthy weight see Healthy weight BMI calculator
Growth Charts: Boys
Boy's head circumference 0–2 years (from page 34 of the Well Child Tamariki Ora My Health Book)

Boy's weight 0–1 year (from page 35 of the Well Child Tamariki Ora My Health Book)

Boy's length 0–2 years (from page 36 of the Well Child Tamariki Ora My Health Book)

Boy's weight 1–5 years (from page 37 of the Well Child Tamariki Ora My Health Book)

Boy's height 2–5 years (from page 38 of the Well Child Tamariki Ora My Health Book)

Growth Charts: Girls
Girl's head circumference 0-2 years (from page 39 of the Well Child Tamariki Ora My Health Book)

Girl's weight 0–1 year (from page 40 of the Well Child Tamariki Ora My Health Book)

Girl's length 0–2 years (from page 41 of the Well Child Tamariki Ora My Health Book)

Girl's weight 1–5 years (from page 42 of the Well Child Tamariki Ora My Health Book)

Girl's height 2–5 years (from page 43 of the Well Child Tamariki Ora My Health Book)

Well Child Tamariki Ora Assessments
- Birth assessment
- 24–48 hours assessment
- First week assessment
- Transfer of care
- 2–6 weeks LMC final assessment
- 4–6 weeks assessment
- 8–10 weeks assessment
- 3–4 months assessment
- 5–7 months assessment
- 9–12 months assessment
- 15–18 months assessment
- 2–3 years assessment
- B4 School Check
NOTE: The assessment pages completed by your health provider and pages for you to complete have not been included here. To see them, please refer to the pages in your copy of the Well Child Tamariki Ora My Health Book, or the PDF (you can download the PDF at the top of the page).
Birth assessment
Completed by your Lead Maternity Carer.
24–48 hours assessment
Completed by your Lead Maternity Carer.
First week assessment
Things to talk about
- Your baby’s feeding; establishing breastfeeding
- Maternal iodine supplements
- Safe sleeping for your baby
- Immunisation information
- Smokefree and vape free baby zone (including in the car)
- Vitamin D supplements for babies at higher risk for low Vitamin D levels (see Vitamin D and your baby)
- Newborn metabolic screening result
- Your baby’s behaviour cues and needs (crying)
- Hearing and vision checklist
- Infant car seat and car safety
- Keeping your child healthy and safe
- Other children’s reactions to baby
- Nutrition for breastfeeding – see Eating for Healthy Breastfeeding Women or search HealthEd for vegan resources
- Coping with stress and fatigue
- Feeling sad, anxious or upset
- Parent/caregiver support and education available
- Early learning in the home
Talk to your Lead Maternity Carer about enrolling with a Well Child Tamariki Ora provider and doctor (see the transfer of care forms on pages 55 to 59).
Registering the birth of your baby
Have you registered the birth of your baby? If not, you need to do this through the Births, Deaths and Marriages section of the Department of Internal Affairs before your baby is two months old. Registering a new baby and getting a birth certificate | New Zealand Government has more information, including how to register online. Birth registration is free. Once registered, and on payment of the fee, a birth certificate is available.
First week assessment
Completed by your Lead Maternity Carer.
See your copy of the Well Child Tamariki Ora My Health Book, or the PDF.
Transfer of care
See your copy of the Well Child Tamariki Ora My Health Book or the PDF for the transfer of care forms. Your Lead Maternity Carer will send these forms to your Well Child Tamariki Ora provider before your baby is a month old.
LMC final assessment (Before the LMC final assessment)
What is your baby doing at 2–6 weeks?
Most babies can see and hear well, but the few who can’t need help as soon as possible. Check your baby’s eyes and ears regularly by going through the questions below, and let your Lead Maternity Carer (LMC) know if you answered ‘no’ to any of the questions. Please be aware, however, that these hearing questions do not replace the hearing screening done around the time of your baby’s birth.
Vision
Can your baby see well?
Do they…
- close their eyes against a bright light?
- stare at people’s faces when they are up close?
- turn towards light?
- smile at you without being touched or spoken to?
Hearing
Can your baby hear well?
When there is a sudden loud noise, do they…
- jump or blink?
- stir in their sleep?
- stop sucking for a moment?
- look up from sucking?
- cry?
What else does your baby do?
Things to talk about
- Your baby won’t have any teeth yet, but it is important to enrol them with the Community Oral Health Service. It’s free.
- Your baby’s feeding
- Your baby’s sleeping
- Safe sleeping for your baby
- Your baby’s behaviour cues and needs (crying)
- Recognising illness
- Stool colour (poos, tūtae) – are your baby’s stools normal yellow/brown in colour or pale like putty?
- Immunisations
- Hearing and vision checklists
- Car seat and car safety
- Smokefree and vape free baby zone (including in the car)
- Keeping your baby healthy and safe
- Other children’s reactions to baby
- Introduction to other parents/caregivers
- Coping with stress and fatigue, sad feelings
- Breastfeeding
- Maternal iodine supplements
- Contraception
- Parent/caregiver support and education services
- Early learning in the home
- Stress, worry, anxiety or postnatal depression
LMC final assessment
Completed by your Lead Maternity Carer.
See your copy of the Well Child Tamariki Ora My Health Book, or the PDF.
4–6 weeks assessment
Before the 4–6 weeks assessment
What is your baby doing at 4–6 weeks?
Most babies can see and hear well, but the few who can’t need help as soon as possible. Check your baby’s eyes and ears regularly by going through the questions below, and let your Well Child Tamariki Ora nurse or doctor know if you answered ‘no’ to any of the questions. Please be aware, however, that these hearing questions do not replace the hearing screening done around the time of your baby’s birth.
Vision
Can your baby see well?
Do they…
- close their eyes against a bright light?
- stare at people’s faces when they are up close?
- turn towards light?
- smile at you without being touched or spoken to?
Hearing
Can your baby hear well?
When there is a sudden loud noise, do they…
- jump or blink?
- stir in their sleep?
- stop sucking for a moment?
- look up from sucking?
- cry?
What else does your baby do?
Things to talk about
- Your baby’s feeding; breastfeeding
- Maternal iodine supplements
- Your baby’s sleeping
- Safe sleeping for your baby
- Your baby’s behaviour cues and needs (crying)
- Recognising illness
- Stool colour (poos, tūtae) – are your baby’s stools normal yellow/brown in colour or pale like putty?
- Protecting your baby through timely immunisation
- Have you enrolled your baby with the Community Oral Health Service?
- Hearing and vision checklists
- Keeping your child healthy and safe
- Car seat and car safety
- Smokefree and vape free baby zone (including in the car)
- Other children’s reactions to baby
- Introduction to other parents/caregivers
- Your feelings about being a parent
- Coping with stress and fatigue, feeling sad or anxious
- Contraception
- Parent/caregiver support and education services
- Early learning in the home
- Stress, worry, anxiety or postnatal depression
- Finally, have you registered the birth of your baby? Go to Registering a new baby and getting a birth certificate | New Zealand Government for information about how to do this, before your baby is two months old.
4–6 weeks assessment
Completed by your Well Child Tamariki Ora provider.
See your copy of the Well Child Tamariki Ora My Health Book, or the PDF.
8–10 weeks assessment
Before the 8–10 weeks assessment
What is your baby doing at 8–10 weeks?
Vision
Can your baby see well?
Do they…
- close their eyes against a bright light?
- stare at people’s faces when they are up close?
- turn towards light?
- smile at you without being touched or spoken to?
Hearing
Can your baby hear well?
When there is a sudden loud noise, do they…
- jump or blink?
- stir in their sleep?
- stop sucking for a moment?
- look up from sucking?
- cry?
What else does your baby do?
Talk to your Well Child Tamariki Ora provider or your doctor if you think your baby is not seeing or hearing well.
Things to talk about
- Your baby’s feeding
- Maternal iodine supplements
- Your baby’s sleeping patterns
- Safe sleeping for your baby
- Your baby’s behaviour cues and needs (crying)
- Social development and play
- Family relationships – the bond between parents/caregivers is important for a baby’s brain development and emotional well-being
- Hearing and vision checklists
- Have you enrolled your baby with the Community Oral Health Service?
- Protecting your baby through timely immunisation
- Recognising illness
- Keeping your child healthy and safe
- Infant car seat and car safety
- Smokefree and vape free baby zone (including in the car)
- Protection from falls
- Protection from choking on small objects
- Hot water/burn protection
- Sunburn protection
- Your feelings about being a parent
- Returning to work outside the home; combining breastfeeding and paid work
- Parent/caregiver support groups and education services
- Early learning in the home
- Stress, worry, anxiety or postnatal depression
Your baby’s development
How is your baby learning and developing?
Think about:
- In what way(s) does your baby move?
- How does your baby show what they want?
- What do you think your baby understands?
- How does your baby act around family members?
- In what way(s) does your baby play?
At your baby’s 3–4 months check, you and your Well Child Tamariki Ora provider will complete a simple questionnaire about your baby’s development. This questionnaire is called PEDS-R, or Parents’ Evaluation of Developmental Status - Revised. It will help you to think about your baby’s development in a number of areas.
8–10 weeks assessment (completed by your Well Child provider)
See your copy of the Well Child Tamariki Ora My Health Book, or the PDF.
3–4 months assessment
Before the 3–4 months assessment
What is your baby doing at 3–4 months?
Vision
Can your baby see well?
Do they…
- close their eyes against a bright light?
- stare at people’s faces when they are up close?
- turn towards light?
- smile at you without being touched or spoken to?
- look at their own fingers?
Hearing
Can your baby hear well?
Do they…
- blink or cry when there is a sudden noise?
- stop crying or sucking when you talk?
- wake or stir to loud sounds?
- coo or smile when you talk?
- turn their eyes towards voices?
- seem to like a musical toy?
- stop moving when there is a new sound?
- seem to know your voice?
Talk to your Well Child Tamariki Ora provider or your doctor if you think your baby is not seeing or hearing well.
When your baby’s teeth start coming, you might like to record their arrival on the teeth diagram (page 32).
Things to talk about
- Your baby’s feeding
- Maternal iodine supplements
- Safe sleeping for your baby
- Your baby’s behaviour cues and needs (crying)
- Social development and play
- Family relationships – the bond between parents/caregivers is important for a baby’s brain development and emotional well-being
- Hearing and vision checklists
- Teething. Have you enrolled your baby with the Community Oral Health Service?
- Protecting your baby through timely immunisation
- Recognising illness
- Smokefree and vape free baby zone (including in the car)
- Infant car seat and car safety
- Protection from poisons
- Protection from falls
- See Keeping your child healthy and safe
- Your feelings about being a parent
- Parent/caregiver support and education services
- Early learning in the home
- Stress, worry, anxiety or postnatal depression
- Returning to work outside the home
- Choices in early childhood education and other learning options and early enrolment
Your baby’s development
Do you have any concerns about your baby’s learning, development and behaviour? In particular, think about:
- how your baby makes sounds
- how your baby uses his or her hands and fingers to do things
- how your baby moves his or her arms or legs
- how your baby gets along with others.
The PEDS-R questionnaire
What is PEDS-R?
PEDS-R stands for Parents’ Evaluation of Developmental Status - Revised.
PEDS-R is a 12-item questionnaire that asks you (the parent or guardian) about your child at specific times before the age of 5 years. Your Well Child nurse will explain how and when to complete the PEDS-R questions.
Why PEDS-R?
As a parent/caregiver, you know your child better than anyone else does. You may notice things about your child that concern you – and even things that no one else has noticed. The PEDS-R questionnaire asks you about any concerns you have about your child and can help pick up any problems early on. Early identification of any developmental problems and support to deal with them can make a big difference.
Sharing any concerns you or your family/whānau have about your child can help your Well Child nurse to work in partnership with you to understand your child better.
3–4 months assessment
Completed by your Well Child Tamariki Ora provider.
See your copy of the Well Child Tamariki Ora My Health Book, or the PDF.
5–7 months assessment
Before the 5–7 months assessment
What is your baby doing at 5–7 months?
Vision
Can your baby see well?
Do they…
- follow a slow-moving, bright-coloured object with their eyes?
- reach out for toys and other things?
- hold them firmly and look closely at them?
Hearing
Can your baby hear well?
Do they…
- turn towards a sound or someone speaking?
- cry when there is a sudden noise?
- like music?
- make lots of different babbling sounds?
- sometimes copy sounds you make?
Talk to your Well Child Tamariki Ora provider or your doctor if you think your baby is not seeing or hearing well.
Things to talk about
- Introducing solids alongside breastfeeding (at around 6 months) – ask for the leaflet Starting Solids (HE6014) and the booklet Eating for Healthy Babies and Toddlers (HE1521) or see the resources from Health Promotion, Health New Zealand | Te Whatu Ora on infant feeding
- Maternal iodine supplements
- Your baby’s sleeping
- Safe sleeping for your baby
- Your baby’s behaviour cues and needs (crying)
- Social development and play
- Family relationships – the bond between parents/caregivers is important for a baby’s brain development and emotional well-being
- Hearing and vision assessments
- Teething, toothbrushing and dental health
- Have you enrolled your baby with the Community Oral Health Service?
- Protecting your baby through timely immunisation
- Recognising illness
- Keeping your child healthy and safe
- Infant car seat and car safety
- Smokefree and vape free baby zone (including in the car)
- Protection from falls
- Protection from choking on small objects
- Hot water/burn protection
- Sunburn protection
- Returning to work outside the home; managing breastfeeding and paid work
- Your feelings about being a parent
- Parent/caregiver support groups and education services
- Early learning in the home
- Choices in early childhood education and other learning options and early enrolment
- Healthy eating from 9-12 months
Your baby’s development
Do you have any concerns about your baby’s learning, development and behaviour? In particular, think about:
- how your baby makes speech sounds
- how your baby understands what you say
- how your baby uses their hands and fingers to do things
- how your baby uses their arms or legs
- how your baby gets along with others
- how your baby is learning to do things for themselves.
5–7 months assessment
Completed by your Well Child Tamariki Ora provider.
See your copy of the Well Child Tamariki Ora My Health Book, or the pdf.
9–12 months assessment
Before the 9–12 months assessment
What is your child doing at 9–12 months?
Vision
Can your child see well?
Do they…
- pick up small things like bits of fluff from the floor?
- follow the movement of a dangling ball in all directions?
- look for dropped toys?
- watch what people are doing near them?
- tilt their head sideways to look at things?
- have a lazy eye, ‘cross’ eye or squint (when both eyes don’t look straight at you most of the time)?
Hearing
Can your baby hear well?
Do they…
- respond to their own name?
- look around to find new sounds – even quiet ones?
- understand ‘no’ and ‘bye-bye’?
- listen when people talk?
- like copying sounds?
- use babbling that sounds like real speech?
- try to talk back when you talk?
Talk to your Well Child Tamariki Ora provider or your doctor if you think your child is not seeing or hearing well.
See the glue ear and earache sections for what to do about these ear problems.
Things to talk about
- Safe sleeping for your baby
- Your child’s play needs
- Reading to your child
- Your child’s nutrition
- Teething and toothbrushing – your child probably has some teeth by now. Have you enrolled them with the Community Oral Health Service?
- Your child’s behaviour
- Recognising illness
- Protecting your child through timely immunisation
- Keeping your child healthy and safe
- Child car seat and car safety
- Protection when walking
- Protection from roads/wandering
- Smokefree and vape free child zone (including in the car)
- Protection from water
- Protection from falls
- Protection from poisons
- Early learning in the home
- Choices in early childhood education and other learning options and early enrolment
Your child’s development
Do you have any concerns about your child’s learning, development and behaviour? In particular, think about:
- how your child talks and makes speech sounds
- how your child understands what you say
- how your child uses their hands and fingers to do things
- how your child uses their arms or legs
- how your child behaves
- how your child gets along with others
- how your child is learning to do things for themselves.
9–12 months assessment
Completed by your Well Child Tamariki Ora provider.
See your copy of the Well Child Tamariki Ora My Health Book, or the pdf.
15–18 months assessment
Before the 15–18 months assessment
What is your child doing at 15–18 months?
Vision
Can your child see well?
Do they…
- pick up small objects with their finger and thumb?
- point to interesting things (like birds)?
- watch everything that is going on around them?
- search with their hands rather than their eyes?
- bring objects up close to their eye?
- have a lazy eye, ‘cross’ eye or squint (when both eyes don’t look straight at you)?
Hearing
Can your child hear well?
Do they…
- point to people and things they know when asked to?
- copy or repeat simple words or sounds?
- understand things like ‘come here’?
- use their voice to get attention?
- say 2 or 3 words?
- listen when people talk?
Talk to your Well Child Tamariki Ora provider or your doctor if you think your child is not seeing or hearing well.
See the glue ear and earache sections for what to do about these ear problems.
Things to talk about
- Feeding your child – ask for the booklets Eating for Healthy Babies and Toddlers (HE1521) and Eating for Healthy Children Aged 2 to 12 (HE1302)
- Immunisation
- Recognising illness
- Teething, dental health and toothbrushing
- Behaviour and needs
- Getting ready for toileting
- Social and play needs
- Early learning in the home
- Choices in early childhood education and other learning options and early enrolment
- Keeping your child healthy and safe
- Protection from roads/wandering
- Smokefree and vape free child zone (including in the car)
- Hot water protection
- Promoting a safer neighbourhood (playgrounds, drains, etc)
Your toddler will probably have about 12 baby teeth by now and can learn to help you brush them, but after you have brushed their teeth first. Don’t wait for teeth problems; take your child for regular check-ups. Any problems can be recognised and treated early and the dental professionals will give you advice about how best to care for your child’s teeth. Call 0800 TALK TEETH, 0800 825 583 to enrol in the Community Oral Health Service. It’s free.
Or visit Caring for your child's first teeth
Your child’s development
Do you have any concerns about your child’s learning, development and behaviour? In particular, think about:
- how your child talks and makes speech sounds
- how your child understands what you say
- how your child uses their hands and fingers to do things
- how your child uses their arms or legs
- how your child is learning to do things for themselves
- how your child behaves
- how your child gets along with others
- how your child is learning preschool skills.
15–18 months assessment
Completed by your Well Child Tamariki Ora provider.
See your copy of the Well Child Tamariki Ora My Health Book, or the pdf.
2–3 years assessment
Before the 2–3 years assessment
What is your child doing at 2–3 years?
Vision
Can your child see well?
Do they…
- recognise small details in picture books?
- hold objects really close to look at them?
- have a lazy eye, ‘cross’ eye or squint (when both eyes don’t look straight at you)?
Hearing and speaking
Can your child hear and speak well?
Do they, by 2½ years…
- do 2 things when asked, like ‘get the ball and bring it here’?
- repeat what you say?
- continually learn new words?
- say simple sentences with 2 or more words in them?
- use many words that non-family members can understand?
Do they, by 3 years...
- speak clearly so that everyone can understand?
- ask lots of 'what or 'why' questions?
Talk to your Well Child Tamariki Ora provider or your doctor if you think your child is not seeing or hearing well.
See the glue ear and earache sections for what to do about these ear problems.
Things to talk about
- Nutrition
- Caring for your child’s teeth and enrolment with the Community Oral Health Service – your child is entitled to free dental care.
- Behaviour and needs
- Social and play needs
- Toilet training
- Keeping your child healthy and safe
- Smokefree and vape free child zone (including in the car)
- Reading to your child
- Participation in early childhood education and other learning options
- Family relationships
Your child’s development
Do you have any concerns about your child’s learning, development and behaviour? In particular, think about:
- how your child talks and makes speech sounds
- how your child understands what you say
- how your child uses their hands and fingers to do things
- how your child uses their arms or legs
- how your child is learning to do things for themselves
- how your child behaves
- how your child gets along with others
- how your child is learning preschool or school skills.
2–3 years assessment
Completed by your Well Child Tamariki Ora provider.
See your copy of the Well Child Tamariki Ora My Health Book, or the pdf.
B4 School Check
Before the B4 School Check
Answer these questions before the B4 School Check (see your copy of the Well Child Tamariki Ora My Health Book, or the pdf). You could also consider sharing the information from this assessment when enrolling your child in school.
Vision
Can your child see well?
Do they…
- point to interesting things (like birds)?
- run into things – high or low?
- bring objects close to their eyes to look at them?
- tilt their head in an unusual way to look at things?
- have a lazy eye, ‘cross’ eye or squint (when both eyes don’t look straight at you)?
Hearing and speaking
Can your child hear and speak well?
Do they…
- tell a long, clear story about things they have done?
- speak well, with only a few sounds wrong, like ‘r' or ‘s’?
- know what things are for (like hat, apple or plate)?
- like books and being read to?
- understand most of what you say?
Has your child had their 4-year-old immunisations?
Talk to your Well Child Tamariki Ora provider or your doctor if you think your child is not seeing or hearing well.
Your child is entitled to free dental care. Have you enrolled them with a dental therapist or oral health therapist?
See the glue ear and earache sections for what to do about these ear problems.
Things to talk about
- Your child’s diet and nutrition
- Behaviour and needs
- Social and play needs
- Positive family relationships
- How you encourage your child’s positive behaviour
- Reading to your child
- Participation in early childhood education/kōhanga reo
- Preparation for school
- Caring for your child's teeth and enrolment with the Community Oral Health Service - your child is entitled to free dental care
- 4-year-old immunisation
- Recognising illness
- Keeping your child healthy and safe
- Toilet training
- Keeping your child's environment smokefree and vape free (including in the car)
- Road and driveway safety
- Promotion of community safety
Your child’s development
Do you have any concerns about your child’s learning, development and behaviour? In particular, think about:
- how your child talks and makes speech sounds
- how your child understands what you say
- how your child uses their hands and fingers to do things
- how your child uses their arms or legs
- how your child is learning to do things for themselves
- how your child behaves
- how your child gets along with others
- how your child is learning preschool or school skills.
Child health questionnaire (to be completed by you)
See pages 110 to 112 in your copy of the Well Child Tamariki Ora My Health Book, or the pdf.
The B4 School Check may be held at a Plunket clinic, marae or doctor’s clinic, a preschool, a kōhanga reo, or other community centre (or at school). It is important you are with your child for the assessment – you know your child best and can tell the nurse or doctor about your child’s development and day-to-day behaviour.
A registered nurse does the B4 School Check, and vision and hearing technicians do the vision and hearing assessment (see the Vision and hearing screening record, page 14).
Your B4 School provider will have a pamphlet about the B4 School check for you to read before you consent to the check. They will also be able to answer any questions you might have.
B4 School Check (to be completed by your B4 School Check provider)
See your copy of the Well Child Tamariki Ora My Health Book, or the pdf.
Learning and growing
-
Your first 6 weeks together
- Ō kōrua wiki tuatahi e ono
- Your time together from 6 weeks to 6 months
- Tō kōrua noho tahi mai i te 6 wiki ki te 6 marama
- Your time together from 6 months to 12 months
- Tō kōrua noho tahi mai i te 6 marama ki te 12 marama
- Your child between 1 and 2 years
- Ko tō tamaiti i waenganui i te 1 me te 2 tau
- Your child between 2 and 3 years
- Ko tō tamaiti i waenganui i te 2 me te 3 tau
- Your child between 3 and 5 years
- Ko tō tamaiti i waenganui i te 3 me te 5 tau
Your first 6 weeks together
Good to know
Getting to know each other
- Spending time with your baby helps them to feel secure and helps their brain develop. Responding in a consistent way to your baby helps them to make sense of their world.
- Spend time talking and singing to your baby.
- Cuddle them and play with them.
- Some parents/caregivers may take a while to bond with their baby, especially if the birth was hard. This is normal and usually comes right over the first few weeks, as you get to know each other.
Keeping your baby healthy
- Breastfeeding is best for your baby.
- If you are giving a dummy or pacifier to your baby, do not dip it in sugar, honey, or sweetened drinks.
- Immunisation helps protect your baby from serious infectious diseases. First immunisation is due at 6 weeks
- A smokefree and vape free home and car helps to protect your baby from asthma and some serious infections.
Keeping your baby safe
- Sleeping your baby on their back and in their own cot, bassinet, wahakura (woven flax bassinet) or pēpi-pod® in the same room as the parents helps protect against SUDI (Sudden Unexpected Death in Infancy).
- Babies don’t need pillows and they are safest sleeping on their backs – this keeps their airway clear for breathing.
- Use a properly installed baby car seat in all cars for all trips. Car seats can be hired.
- Always take your baby with you when you leave the car.
- Test that bathwater is not too hot for your baby.
- Never shake, hit or smack your baby – if you feel you might lose control, put them in a safe place and walk away for a short time. See Coping with a crying baby
Looking after yourself
- Ask for and accept offers of help.
- Talk to family/whānau, friends, neighbours.
- Find parent/caregiver support groups that suit you.
- If you often feel sad, anxious and unable to cope, talk to someone you trust.
Check Keeping your child healthy and safe.
Ō kōrua wiki tuatahi e ono
He pai ki te mōhio
Te mōhio haere ki a kōrua anō
- Mā te noho tahi me tō pēpi ka āwhina kia noho pai ia me te whakawhanake i tōna hinengaro.
- Me whai wā koe ki te kōrerorero me te waiata ki tō pēpi.
- Awhitia tō pēpi, tākaro tahi ki a ia.
- Ka roa ake pea te wā mō ētahi mātua ki te hono ki tā rātau pēpi, otirā mēnā i tino uaua te whakawhānau. He tikanga tonu tēnei, ā, ka pai haere i roto i ngā wiki tuatahi, e mōhio haere ai kōrua ki a kōrua.
Te tiaki kia ora tō pēpi
- Ko te whāngai ū te mea pai rawa mō tō pēpi.
- Mēnā kai te hoatu e koe he tami, he whakarata rānei mā tō pēpi, kaua rawa e tautau ki te huka, mīere, ētahi atu waireka rānei.
- Ka āwhina te ārainga mate kia noho haumaru tō pēpi mai i ngā mate hōrapa taumaha (kei te wiki tuaono te ārainga mate tuatahi, tirohia Te Ārainga Mate).
- Ka āwhina te kāinga me te waka auahi kore, rehutupeka kore hoki ki te tiaki i tō pēpi mai i te mate huangō, me ētahi atu mate taumaha.
Kia haumaru tō pēpi
- Te whakatau i tō pēpi kia takoto ia ki tōna tuara moe ai ki roto anō i tōna ake moenga, wahakura, pēpi-pod® rānei i te rūma moe o ngā mātua hei pare atu i te mate kōhungahunga pā whakarere noa (SUDI).
- Hei aha he urunga mō te pēpi, ā, he pai ake tana takoto i runga i tōna tuara – ka noho wātea tōna arahau mō te hehē.
- Whakamahia he tūru waka kōhungahunga mō ngā haerenga katoa. Me mātua whakarite kei te mau tika te tūru waka kōhungahunga o tō pēpi i roto i tō waka mō ia haerenga. Ka taea ngā tūru waka te rīhi.
- Me heri koe i tō pēpi i ngā wā katoa ka wehe ana koe i tō waka.
- Whakamātauria te wai horoi kia kore ai e tino wera rawa mō tō pēpi.
- Kaua rawa e rurerure, e patu, e papaki rānei i tō pēpi – mēnā ki tō whakaaro ka keka koe, me waiho te pēpi ki tētahi wāhi haumaru ka hīkoi atu mō tētahi wā poto. Tirohia Te tū pakari me tētahi pēpi tangitangi
Te tiaki i a koe anō
- Me tono āwhina, me te whakaae ki ngā whakaaro āwhina.
- Kōrero ki tō whānau, ō hoa, kiritata hoko.
- Kimihia ngā rōpū mātua tautoko e hāngai ana ki a koe.
- Mēnā he rite tonu tō noho pōuri, mānatunatu me tō kore noho tau, me kōrero koe ki tētahi tangata e pono ana koe.
Tirohia Kia haumaru, kia ora tō tamaiti
Getting to know your new baby
Spend time with your baby to develop your bond
Cuddling your baby, singing to them and giving them attention helps their brain to develop and makes them feel secure. It also helps you to get to know your baby, feel comfortable and relaxed with them, and enjoy them.
To grow and develop as a person, a baby needs smiles, laughter, touch, and interaction just as much as food or sleep. Your body language, tone of voice, and loving touch are all important ways of communicating with your baby.
Mothers need to look after themselves too
Becoming a mother is like nothing else you’ll ever do. Becoming a parent is a big change in your life. This is a time when you discover feelings you didn’t know you had. It’s very exciting but it can also be scary. To look after your baby well you need to look after yourself too. Your baby needs you to be happy and healthy!
That means getting the sleep you need. Rest when your baby is asleep. Make sure you are eating well. Drink whenever you are thirsty, especially if you are breastfeeding.
Do try not to do too much too soon. Housework is not as important as you and your baby. Ask for help from family/whānau, friends and neighbours.
Share your feelings with your partner, family/whānau, a good friend, your Lead Maternity Carer, Well Child Tamariki Ora nurse or doctor.
Breastfeeding is best for your baby
Breast milk is all your baby needs to eat and drink for about the first 6 months.
Breastfed babies get sick less often. Breast milk is more than a food. It also helps to improve immunity to illness – it can provide some protection against a range of infections, especially ear, stomach and respiratory infections in childhood and against diabetes and obesity in adulthood.
How long should I breastfeed?
It is best to feed your baby only breast milk until they are ready for and need extra food (around 6 months of age). If you can, continue to breastfeed until 2 years of age or beyond. Breastfeeding and the close physical contact with your baby is important over the first months to create a strong bond in the baby’s first important relationship. This helps the pathways in your baby’s brain to develop properly.
Getting started
Most women can breastfeed. Many women need help when they begin breastfeeding, especially with their first baby. Mothers and babies learn to breastfeed together.
It can take up to 6 weeks to fully establish breastfeeding. Your midwife will help you get started and so will the midwives and lactation consultants working in the hospital where you give birth. Ask for help when you need it. Other breastfeeding women can be very helpful and a support group can help as you move beyond the newborn stage.
Be patient as you and your baby learn to breastfeed. Feed your baby as soon as possible after birth. Ask your midwife to be with you for the first feed, to help with the best position and latch for your baby in order to get your milk supply going and to prevent sore nipples. Skin to skin contact with you after birth is good for your baby’s physical health and helps you bond with each other.
If your baby has ongoing trouble latching on, talk to your midwife, Well Child Tamariki Ora nurse, or a lactation consultant.
Breastfeeding takes a lot of time at first and most new babies want to feed often. Make sure you get plenty of rest – sleep when your baby does and get help from your family, whānau and friends with household chores and childcare if you have other children.
Ask your midwife, nurse or doctor to help your baby feed effectively. If you feel you have a problem with breastfeeding, are worried about your milk supply, or find feeding painful, ask for help. They can provide you with information and support before and after the birth and may refer you to a lactation consultant. Hospitals run breastfeeding workshops for new mothers. Breastfeeding groups such as La Leche League also provide help.
If you feel tired and unwell, and part of your breast feels sore, hot or lumpy, see your midwife, nurse or doctor. You may have inflammation caused by a blocked milk duct (this is called mastitis). If this happens, it doesn’t mean you need to give up breastfeeding.
Keep feeding your baby from the affected breast first, massaging the sore area gently at the same time. Emptying the breast will help reduce the blockage and keep your milk flowing. It is important that you rest. Keeping the sore area warm with a wheat pack or wrapped hot water bottle will help you feel more comfortable. Your doctor may prescribe some medicine to reduce the inflammation, but this is not usually necessary.
Your milk supply
Build up your milk supply by letting your baby feed as often and for as long as they want. From time to time your baby will need to feed more than you expect. This does not mean you are running out of milk – it’s your baby’s way of encouraging you to make more milk for them as they grow. After a few days of extra feeds your milk supply will grow to meet your baby’s needs. Breastfed babies who are well do not need other fluids.
How do I know my baby is getting enough milk?
Babies who are getting enough milk gain weight, are well and mostly happy, and have 6 to 8 washable nappies or 5 to 6 disposable nappies a day, with urine that is a pale yellow colour.
Your baby is satisfied and feeling full when they:
- release the breast and can be moved away without being unlatched
- look relaxed and contented
- look very sleepy and extend their legs
- have stopped showing signs of restlessness or hunger
Eating for breastfeeding
You do not need to eat any special foods while breastfeeding, but it is a good idea for you to eat a healthy diet (just like everyone else). If you are a vegetarian, a well-balanced diet should make sure you and your baby get all the nutrients you both need. If you are a vegan, you may need extra supplements – consult your midwife, Well Child Tamariki Ora nurse or doctor.
Iodine is an essential nutrient. Requirements for iodine increase during pregnancy and breastfeeding. Take one 150 microgram iodine-only tablet daily when breastfeeding. This can be purchased at pharmacies (or at a lower cost, when prescribed by your doctor, nurse practitioner or midwife).
Eating spicy or ‘gas-producing’ foods (such as beans or cabbage) is usually fine – there are no foods that bother all babies. You may only need to avoid a certain food if your baby is unsettled, cries a lot or has gas every time you eat it. Please talk to your health professional if you have any concerns.
Ask for the free booklets Breastfeeding Your Baby – English version - HE2098 – HealthEd (also available in other languages) and Eating for Healthy Breastfeeding Women/Ngā Kai Totika mā te Ūkaipō – HealthEd
Useful websites
The Health New Zeland | Te Whatu Ora website has a large and helpful section on Breastfeeding. This section covers how to breastfeed, advice on common problems with breastfeeding, breastfeeding at work and supporting a breastfeeding parent. The Plunket website is also very helpful – see Feeding » Whānau Āwhina Plunket).
If you are not breastfeeding
Use an infant formula designed specially for young babies, not cow’s milk. Cow’s milk is not suitable for babies under 12 months because it does not have enough iron or vitamin C and can irritate the bowel. Babies need iron to grow and develop; without enough iron they may become anaemic, which makes them unsettled and can slow their development.
Feeding equipment (including any items used with breast milk) must be washed and sterilised until your baby is at least 6 months old and thoroughly washed and rinsed once your baby is over 6 months. From birth until your baby is at least 6 months old, water used for formula must be boiled and cooled on the day you use it. From 6 months of age you can use water straight out of the tap to make formula.
Always wash your hands before preparing formula feeds.
Follow the instructions on the formula can or packet carefully. Use the scoop provided and do not add more water or powder than directed. In rural areas, water may contain nitrates, which are dangerous for your baby. Water from a private supply (such as from a well or bore) should be boiled and cooled until the infant is 18 months old. It is recommended to have water from a private supply tested for any contaminants that could harm a baby. If testing shows water is high in nitrates, it is not suitable for preparing infant formula. (Boiling does not remove nitrates.) Use the formula as soon as possible after it is prepared and throw any leftover formula away after 2 hours.
You don’t need to warm your baby’s formula. Babies don’t mind it at room temperature, especially if the weather is hot. If you do warm your baby’s formula, the safest way to warm formula is by placing the bottle in a container of hot water. Microwaves are not recommended for warming bottles because they can overheat the formula or heat it unevenly and burn your baby’s mouth.
Shake any warmed formula well and always check the temperature by testing some on your wrist. It should feel about the same heat as your skin. If it feels hot, leave it to cool down before feeding your baby.
If you are travelling with your baby, measure the correct amount of water for one feed into a cleaned and sterilised bottle. Don’t add the powder until you are about to feed your baby.
For more information, see the booklet Feeding Your Baby Infant Formula (HE1306).
Ask your Lead Maternity Carer or Well Child Tamariki Ora nurse about sterilising bottles and teats.
See Safe drinking water for your baby’s feeds or phone PlunketLine 0800 933 922.
Useful websites
Formula Feeding | KidsHealth NZ has useful information about formula feeding, including videos about feeding choices.
Vitamin D and your baby
Vitamin D helps our bodies use calcium to build and maintain strong bones. Our bodies can make it from the sun. However, babies can’t safely get the vitamin D they need from the sun. Their skin is very sensitive and should not be exposed to direct sunlight. See Sensible sun exposure
Low levels of vitamin D in babies and children can cause rickets. Rickets can result in weak bones, delayed walking, bowed legs, and swollen wrists or ankles. If untreated, rickets can lead to failure to grow, deformed or broken bones, pneumonia and seizures.
Breast milk is the ideal food for your baby but it may not give them all the vitamin D they need. Supplements can be given to babies who have a high risk of vitamin D deficiency.
When is there a high risk?
Your baby needs vitamin D if your baby is breastfed and:
- has naturally dark skin
- you have been told that you are low in vitamin D
- one or more of your other children has had rickets or seizures resulting from low levels of calcium in their blood.
Babies who are born early and have a low body weight may be vitamin D deficient.
Babies who are breastfed over winter months in New Zealand may also be vitamin D deficient by late winter or spring.
Supplements for babies at risk of deficiency
If your baby is at high risk of vitamin D deficiency, talk to your Lead Maternity Carer, Well Child Tamariki Ora provider, doctor, or a dietitian. Your doctor can prescribe a vitamin D supplement that comes in drops.
For more information, go to Vitamin D & Your Baby | KidsHealth New Zealand's Trusted Voice On Children's Health
Bathing your baby
How often you bathe your baby is up to you. Once or twice a week will keep a newborn baby clean. Between baths, wash your baby’s face regularly and clean their bottom at every nappy change.
Most babies love being in the water, and bath time can be a fun and relaxing experience you can both enjoy.
If you do not have a bath, you can wash them in a large basin or while they lie on a towel. It may be helpful if someone else is there to give you a hand. Holding a wet and wriggling baby can feel scary when you are not used to it!
Put cold water in your baby’s bath first, then add the hot water. Test the heat of the water before you put your baby in; it should be about 37°C. One way to check is to put the inside of your wrist in the water.
Slip your arm under your baby’s back and hold their arm that is away from you with your hand. Then with your free hand or a soft cloth wash their body, ensuring that their face is held out of the water.
Never leave your baby alone in the bath, even for a second. You can’t rely on bath seats or mats to keep your baby or toddler safe. If you need to go away, take your baby with you, or make sure another adult is with them. Never leave babies in the care of other children in the bath – they might not react as quickly as an adult if your baby slips under the water.
Bath time is also a chance for other members of the family/whānau to spend time with the baby. Fathers/partners often enjoy this as a special time to spend with their children.
A smokefree and vape free home and car help protect your baby from disease
Cigarette smoke is very harmful for your baby, both during pregnancy and after birth. Babies who live with smokers get sick more often.
The arrival of a baby is a good reason to stop smoking. There are better ways to quit so you can kick the smokes for good. You can:
- check out the tips at Supporting Aotearoa to live and breathe smokefree | Smokefree.org.nz
- call Quitline 0800 778 778
- get a free Quit Coach – Find a stop smoking service | Smokefree.org.nz
- ask your midwife, Well Child Tamariki Ora nurse or doctor about smokefree
programmes near you.
In addition to the the health benefits of quitting, you'll save a ton of money (if you smoke 15 cigarettes a day, you can expect to save over $9,000 a year). Check out how much money you could be saving at Smoking cost calculator | Smokefree.org.nz
What about vaping?
Vaping is not harmless, but is likely to be less harmful than smoking while pregnant or breastfeeding.
As vaping is relatively new we do not know how dangerous second-hand vapour is to others. However it is best to not vape around children, especially in confined spaces like your car.
For more information on vaping visit Vaping Facts
You can find more information on the Smokefree website
Protect your baby against Sudden Unexpected Death in Infancy (SUDI)
Sudden Unexpected Death in Infancy (SUDI) is a risk to babies until they are about 12 months old.
Although for some babies the cause of death is never found, many of these deaths are caused by suffocation and are preventable. There are things we can do to protect our babies.
Make every sleep a safe sleep
Review your baby’s sleep environment with your midwife during your first week at home. This will help you to be sure that your baby has their own safe sleep space – usually a cot or bassinet in the first few months (see the First week assessment).
Always follow these safe sleep routines for your baby and your baby’s cot.
Make sure your baby is safe
Sleep your baby on their back to keep their airways clear for breathing. Put your baby to sleep in their own cot, not with an adult or another child who might accidentally smother them.
Always make sure your baby has a parent/caregiver who is alert to their needs and free from alcohol or drugs. Just as you would nominate a sober driver, every baby and child needs a sober caregiver.
Make sure your baby sleeps in their own bed
The safest place for all babies to sleep at night is in their own bed, bassinet, pēpi-pod® or wahakura, close to parents/caregivers and in the same room.
If you choose to sleep in bed with your baby, it is much safer to put them in their own baby bed – for example, a pēpi-pod® or wahakura – beside you. This may help reduce the risk of your baby suffocating while they are asleep.
If you are out somewhere, make sure your baby has a safe place to sleep. Take your wahakura, pēpi-pod®, cot or bassinet with you.
It is never safe to put your baby to sleep in an adult bed, on a couch or on a chair.
Car seats or capsules protect your baby when travelling in the car. They are not suitable for your baby to sleep in when you are at home or at your destination.
If you don’t have a baby bed, ask your Lead Maternity Carer or child health nurse for assistance to get one. If you are on a low income, you may be able to receive help from Work and Income.
For more information visit Work and Income or call 0800 559 009
Make sure your baby’s bed is safe
Your baby’s bed needs a firm flat mattress that fits snugly so your baby can’t get into any gaps between the frame and the mattress. There should be nothing in the bed that could cover their face or lift their head – no large stuffed toys, pillows, loose bedding or bumper pads. Babies don’t need pillows and are safest sleeping flat on their backs.
Make sure your baby is healthy and strong
Being smokefree during pregnancy and after is best for your baby. If a mother smokes during pregnancy, poisonous chemicals affect the growing baby. This weakens them after they are born so that they are unable to react as strongly to situations such as accidentally having their face covered. After your baby is born it is important to keep your home and car smokefree and vape free and make sure that others don’t smoke around the baby. This will help your baby grow strong and healthy.
Feed your baby only breast milk for the first 6 months and when you have introduced solids keep breastfeeding for the first year and beyond. Make sure your baby is immunised on time.
For more on safe sleep, see Protecting your baby from SUDI.
If you find your baby not breathing, call for help, and begin rescue breathing (CPR) immediately.
Head shape
A baby’s head changes shape due to pressure on their soft skull when their head rests on the same spot for long periods. This can happen in all sleep positions because babies have heavy heads and sleep a lot.
To avoid a flat spot developing when your baby is sleeping, turn their head so that they sometimes face left and sometimes face right. Or if you notice they like to face a window, turn them around in their bed to encourage them to move their head to the other side. Giving your baby time upright and on their tummy when they are awake will also help prevent a flat spot from developing.
If you have concerns about your baby’s head shape, talk to your Well Child Tamariki Ora nurse or doctor.
The Change for our Children website has a brochure Protecting Your Baby’s Head Shape.
Coping with a crying baby
Babies can be unsettled for the first few months as they learn to communicate their needs to you. Babies don’t cry because they are being naughty.
Crying often means hunger, a dirty or wet nappy, or they may just need a cuddle, a song, a walk or a ride to soothe them. Carrying your baby in a safe sling will also help settle them. Watch for their responses to your care and learn what works for your baby.
Crying can mean your baby is unwell
If your baby’s cry is unusual – such as piercing and high pitched – take them to a doctor straight away (see Danger signs on the back cover).
When a baby cries and cannot be comforted easily, the problem could be what is called ‘colic’. Colic usually happens in the afternoon or evening or after a feed, and it can be very upsetting. No one really knows what causes colic and it usually disappears after the first 3 months. If you think your baby is crying a lot, talk to your Well Child Tamariki Ora nurse or doctor.
When your baby keeps on crying
One of the hardest times can be when your baby keeps on crying and you can’t work out why. If you find yourself getting frustrated or distressed, it is OK to put the baby down gently in a safe place, walk away and take a break. Do not pick up the baby until you have calmed down. Your baby is more likely to calm down when you are feeling calm and in control.
Look after yourself. Make a cup of tea or coffee, phone a friend or someone in your family/whānau.
You could also phone PlunketLine 0800 933 922 or Healthline 0800 611 116 for advice or support.
Never, ever shake a baby. Never leave a baby alone with anyone who may lose control. A single moment of losing control may damage a baby forever. Babies can die if they are shaken.
If you ever think your baby has been hurt, call 111. Don’t let fear or pride stand in your way. It could save your baby’s life.
KidsHealth has a video for parents/caregivers about how to cope with the stress of a child’s crying and the consequences of shaking a baby. It's called 'Power to Protect' and you can watch it at kidshealth.org.nz/never-ever-shake-baby
Getting help and advice
Phone PlunketLine 0800 933 922 or Healthline 0800 611 116 for advice and support. Young parents may like to phone Youthline on 0800 376 633
You can also find helpful information on Kidshealth
Barnardos (see the website or phone 0800 BARNADOS (0800 227 627) or 0800 KIDSTART (0800 543 782) also offers family support and counselling.
When will your baby sleep?
Newborn babies have varied sleep patterns and in the beginning do not know the difference between day and night time. In the first 3 to 6 months many babies wake to feed at least once or twice in the night, but this can vary greatly. From 6 months of age many babies settle into a pattern of having morning and afternoon naps, but often reduce their morning nap as they get more active. Their sleep cycles are shorter than those of adults, with a mixture of light and deep sleep.
A tired baby will rub their eyes, grizzle, yawn, have poor eye contact or stare into space. They may clench their fists, have tense movements and startle more easily than usual.
If night feeds are quiet with no playing, it helps your baby learn the difference between day and night time and develop sleeping habits to match the rest of the family.
Sleep your baby on their back so they can’t roll over onto their face.
Check that your baby is warm but not too hot. The back of their neck or their tummy (under the clothes) should feel warm, not hot or cold. Your baby will be comfortable when their hands and feet are a bit cooler than the rest of their body. Don’t over-wrap your baby or leave them in a closed room with a heater going. Babies can’t throw their blankets off if they get too hot, and overheating can lead to serious illness.
Talk to your Lead Maternity Carer or Well Child Tamariki Ora nurse if you are not sure about what to do.
Many parents/caregivers find that sleeping a baby in the baby’s own bed in the parents’ bedroom makes care easier. It also helps protect against SUDI and overheating.
Sleep recommendations
- Babies (birth to three months) should have 14 to 17 hours good quality sleep every day, including daytime sleeps centred round their physical and emotional needs.
- Infants (four to twelve months) should have 12 to 15 hours good quality sleep every day, including daytime sleeps, which will tend to decrease as they get closer to one year of age.
- Toddlers (one to two years inclusive) should have 11 to 14 hours of good quality sleep every day, including at least one daytime sleep.
- Preschoolers (three to four years inclusive) should have 10 to 13 hours of good-quality sleep every day, with consistent bedtimes and wake-up times.
- For more information see the Active Play Guidelines for Under-Fives
Car seat
You will need a car seat from the day your baby is born. Car seats can be hired from some Well Child Tamariki Ora providers and some retail outlets – ask your Lead Maternity Carer for information. You can also go to Child Car Seats | KidsHealth NZ for advice on purchasing and fitting car seats or Requirements for using child restraints in New Zealand | NZ Transport Agency Waka Kotahi (nzta.govt.nz)
Your time together from 6 weeks to 6 months
Good to know
Getting to know each other
- Spend time talking and singing to your baby.
- Breastfeeding and cuddling your baby helps them feel loved and secure.
- When your baby is awake, watch them have some play time on their tummy.
- Routines for bedtime and bath time help them feel secure.
Keeping your baby healthy
- Breastfeeding helps protect your baby’s health.
- Immunisation helps protect your baby from serious infectious diseases (due at 6 weeks, 3 months and 5 months).
- A smokefree and vape free home and car helps protect against Sudden Unexpected Death in Infancy (SUDI), ear and chest infections and meningitis.
Keeping your baby safe
- Sleeping your baby flat on their back – no pillow – and in their own bed helps protect against SUDI.
- Use properly installed baby car seats in all cars for all trips.
- Test that tap-water temperature is around 50°C.
- Test that bathwater and drinks are not too hot for your baby.
- Keep small toys and objects away from your baby to prevent choking.
- Never shake, hit or smack your baby – if you feel you might lose control, put them in a safe place and walk away for a short time (See Coping with a crying baby).
Looking after yourself
- Ask for and accept offers of help.
- Talk to family/whānau, friends, neighbours.
- Find parent/caregiver support groups that suit you.
- If you often feel sad, anxious and unable to cope, talk to someone you trust.
Tō kōrua noho tahi mai i te 6 wiki ki te 6 marama
He pai ki te mōhio
Te mōhio haere ki a kōrua anō
- Me whai wā ki te kōrero me te waiata ki tō pēpi.
- Mā te whāngai ū me te awhiawhi ka rongo tō pēpi i te aroha, i te tītina.
- I te wā e oho ana tō pēpi, me mātaki i a ia e tākaro ana i runga i tōna puku.
- Mā ngā whakaritenga mō te wā moe me te horoi ka āwhina kia tītina ia.
Te tiaki kia ora tō pēpi
- Ka āwhina te whāngai ū ki te tiaki i te hauora o tō pēpi.
- Ka āwhina te ārainga mate ki te tiaki i tō pēpi mai i ngā mate hōrapa taumaha (hei te 6 wiki me te 3 marama me te 5 marama).
- Ka āwhina te kāinga me te waka auahi kore, rehutupeka kore hoki ki te tiaki i tō pēpi i te mate kōhungahunga (SUDI), ngā whakapokenga taringa me te uma, me te kiriuhi ua kakā.
Kia haumaru tō pēpi
- Kia papatahi te takoto o tō pēpi ki tōna tuara – kaua he urunga – ka mutu ki roto anō i tōna ake moenga hei ārai atu i te mate kōhungahunga.
- Whakamahia he tūru waka kōhungahunga mō ngā haerenga katoa i rō waka.
- Whakamātauria kei te takiwā o te 50°C te pāmahana o te wai o te kōrere.
- Whakamātauria kāore i te tino wera rawa te wai horoi me ngā inu mā tō pēpi.
- Whakawāteahia ngā taputapu tākaro me ngā mea iti mai i tō pēpi kia kore ai e raoa.
- Kaua rawa e rurerure, e patu, e papaki rānei i tō pēpi – mēnā ki tō whakaaro ka keka koe, me waiho te pēpi ki tētahi wāhi haumaru ka hīkoi atu mō tētahi wā poto. Tirohia Te tū pakari me tētahi pēpi tangitangi
Tirohia Kia haumaru, kia ora tō tamaiti
Te tiaki i a koe anō
- Me tono āwhina, me te whakaae ki ngā whakaaro āwhina.
- Kōrero ki tō whānau, ō hoa, kiritata hoki.
- Kimihia ngā rōpū mātua tautoko e hāngai ana ki a koe.
- Mēnā he rite tonu tō noho pōuri, mānatunatu me tō kore noho tau, me kōrero koe ki tētahi tangata e pono ana koe.
Getting to know each other
Cuddling, rocking, talking and singing are some of the ways you can communicate with your baby. Move with your baby to music, to introduce them to rhythm.
When your baby makes sounds, repeat the sounds back so they learn to talk with you. Babies are learning language from birth – talk and sing to them in your own language. Play simple games like peek-a-boo. Point out and name things that can be seen and heard. Talk about what you are doing and make eye contact with your baby while you are talking. Read books to your baby and describe the pictures.
Spending time with your baby grows your relationship with them. Making them part of the patterns of family/whānau life helps you get to know them and they begin to learn what to expect from others. You will learn to recognise the signs that they are tired, or hungry, or need a nappy change and develop routines for bedtimes and bath times. By responding to each other in these kinds of ways, you develop a growing relationship that helps your baby to feel loved and secure.
Feeding your baby
Breastfeeding is still best for your baby. If you are not breastfeeding, keep using an infant formula until they are 12 months old.
Your baby may need extra drinks of breast milk or formula in hot weather and when they are ill. Babies under 6 months of age should not be given water to drink.
If you need to return to the workplace while breastfeeding, Health New Zealand | Te Whatu Ora has advice to support you at Breastfeeding and returning to work
If your baby has diarrhoea, follow the advice in the Diarrhoea and vomiting section. If you are worried, phone Healthline 0800 611 116
Your baby will probably not need solids until about 6 months old.
It’s important not to introduce solid food too early because your baby gets all the nutrition they need from breast milk.
Starting your baby on solid food will not necessarily help them to sleep better at night.
Your baby may start putting their hands or toys in their mouth, or have a growth spurt and want to feed more at around 3 months. This is normal – this does not mean they are ready for solids.
If your baby seems hungry after breastfeeding before they are 6 months old, talk to your Well Child Tamariki Ora nurse or doctor, or ring PlunketLine on 0800 933 922
See Feeding your baby for more about first foods.
Protecting your baby from SUDI
Help protect your baby against Sudden Unexpected Death in Infancy (SUDI).
SUDI is not common, but is a risk to babies during their first year of life.
Although for some babies the cause of death is never found, most SUDI happens when a baby is sleeping in an unsafe way. The commonest cause is suffocation by their bedding or accidental smothering by an adult or child who is sleeping with the baby.
Most of these deaths can be prevented. SUDI is extremely rare when babies are put to sleep in safe sleep conditions. There are many easy things we can do to protect our babies.
The safest place for all babies to sleep at night is in their own cot, bassinet, pēpi-pod® or wahakura, close to parents/caregivers and in the same room.
You can help protect your baby from dying suddenly in their sleep by:
- making sure your baby is in their own bed for every sleep (and in the same room as parents/caregivers at night)
- making sure your baby is on their back for every sleep
- keeping your baby smokefree and vape free from the start
- breastfeeding your baby
- immunising your baby on time.
For more information, see Protecting your baby from SUDI.
Keeping your baby’s bed safe
Babies may begin to roll over from their back to their front when they get to 5 or 6 months old. You don’t need to try and stop this from happening, as long as their cot is free of things that might suffocate them such as pillows, large soft toys or cot bumpers.
Make sure that cots are assembled correctly. The tops on the corner posts of wooden cots may need to be sawn off so your child can’t hang themselves by their clothing. Consumer Affairs New Zealand state that spaces between the bars of the cot must be between 50 mm and 95 mm. Find one with the spaces closer to 50 mm if you can. Make sure the mattress fits well, with no gaps between the mattress and the sides or base of the cot.
The cords for blinds and curtains are a danger. Put the cot away from the window so your child can’t reach them.
For more on preventing choking and strangling, see Choking, strangling, suffocating
Head shape
A baby’s head changes shape due to pressure on their soft skull when their head rests on the same spot for long periods. This can happen in all sleep positions because babies have heavy heads and sleep a lot.
For advice on avoiding a flat spot developing on your baby’s head, see Head shape
Crying
All babies cry. Some cry more than others, especially when they are between 6 weeks and 3 months old. It is very normal for babies at this age to seem unsettled at some time during the day or evening. This can be very stressful, and you may worry that there is something wrong.
If crying makes you angry or upset, ask for help.
Phone a friend for a chat if there is no help at hand, or your Well Child Tamariki Ora nurse, or doctor, PlunketLine 0800 933 922 or Healthline 0800 611 116
Keep trying to get help until you make contact with someone, somewhere. If you feel you might lose control and have no phone, put your baby in a safe place and walk away for a short time (see Coping with a crying baby).
Stress, worry, anxiety or postnatal depression
Becoming a parent is an exciting time. It can also ramp up any stress, anxiety or old trauma. It's thought that up to half of all parents may have low mood or feel distressed after having a baby. Between 10 and 20% of māmā (and up to half of their partners) may feel low enough to be diagnosed with depression or anxiety at some point after pēpi is born.
Experiencing mental or emotional distress and seeking support does not mean that you have ‘failed’ as a person or a parent. It only means you are doing what is most important to your pēpi - making every effort to be well. It is treatable and getting support early leads to the best outcomes.
Mental distress, including anxiety and depression, can be more likely if you or a close family member have experienced these or similar difficulties in the past, or during pregnancy. Stress, loneliness, isolation, lack of support (practical and emotional), a difficult or premature birth, challenges with breastfeeding, relationship issues or violence, or the birth of a pēpi with serious health problems can also contribute to feeling low.
You may feel worthless, hopeless and/or sad and have changes in your eating and sleeping patterns. You may blame yourself when things go wrong, feel anxious, panicky or overwhelmed, and in more severe cases have thoughts of suicide or hurting your pēpi. You might not feel close to your pēpi or to other whānau members. Sometimes these feelings can emerge suddenly and unexpectedly. At other times, your moods may swing for no obvious reason. If these feelings don’t go away in a few days or if you or your whānau are worried about how you feel, talk straight away to your Lead Maternity Carer, Well Child Tamariki Ora nurse, doctor or someone you trust. They will be able to help you, and/or seek help on your behalf.
Partners and other support people need to know what to do if they are worried about your mental health. They should understand that it’s OK to ask for advice about the best way to support you. Talk to other people as well. You may be surprised by how many of your friends and family have had similar feelings when they have had a new baby. Support and practical assistance (meals, childminding, and housework) from family/whānau and friends will help with day-to-day needs and remind you that you are not dealing with this alone. Home help may be another option.
If you are talking to someone, you may want to take a support person with you. Your preferred provider will be able talk to you about treatment such as counselling or in some cases medication. They will also know what help is available in the community, such as postnatal depression groups, community mental health services, home help and counselling.
If you’re worried about postnatal depression or mental or emotional distress talk to your doctor, midwife, Well Child Tamariki Ora provider or someone you trust. Or alternatively you can call:
- Healthline 0800 611 116
- Plunketline 0800 933 922 or visit a local Plunket Family Centre (to find one, see Plunket near me on Home » Whānau Āwhina Plunket). You don't have to be using Plunket to use this phone line.
- If you want to talk (kōrero) to a trained counsellor about how you’re feeling, or you’ve got any questions, you can call the Depression Helpline 0800 111 757 or Need to talk? Free call 1737 or free text 1737 any time for support from a trained counsellor.
For more information on mental distress during pregnancy or after your pēpi is born, you can visit:
- PADA - Perinatal Anxiety & Depression Aotearoa
- National Depression Initiative: Navigating parenthood | Depression and Anxiety | Welcome to a Brand New Day or There is a way through: A guide for people experiencing stress, depression
- Mental Health Foundation
Alcohol and other drugs can make your depression worse.
Teething
Teeth start growing before a baby is born. Your baby’s first tooth doesn’t usually show until about 5 or 6 months after birth, and the last one at about 2½ years. The bottom front teeth usually come through the gum first.
Most babies don’t show any distress when their first teeth come through, but for some, the gums swell and become sore as teeth break through. Teething may also be associated with restlessness and crying, a slight fever, cheek redness, not eating or sleeping well, drooling and a desire to bite something hard.
What you can do
If your baby is upset, gently rub their gums with a clean finger or the back of a cold spoon. You can also apply ice cubes wrapped in a wash cloth to the reddened cheek. Your pharmacy has special teething lotions and gels to gently massage into the gums.
Give something to chew on, such as a clean teething ring. It is best to avoid teething rings that have liquid inside, as the liquid may not be safe if the ring breaks.
If your baby has a lot of pain, has bleeding or pus in their gums or swelling in the mouth or face, get help from a doctor or nurse or call Healthline 0800 611 116. Or contact a dental or oral health therapist at the Community Oral Health Service 0800 TALK TEETH, 0800 825 583
Teething does not make babies sick and does not cause high fever, vomiting, diarrhoea or ear infections. If your baby is unwell, check with your Well Child Tamariki Ora nurse or doctor (ring Healthline 0800 611 116 if you can’t get to a doctor easily).
Looking after your baby’s first teeth
Teeth are at risk of dental decay from the time they start to appear. From about 6 months of age children are at risk of tooth decay.
To keep teeth healthy you should start to brush your baby’s teeth as soon as they come through the gum. Use a small soft brush and half a pea-sized amount of regular-strength fluoride toothpaste twice a day. One brushing should be last thing at night before bedtime. Use 1000 ppm (regular strength) toothpaste – only half a pea-sized amount for younger children. This is based on many years of research on the effectiveness of different strength toothpastes. (See the fluoride toothpaste section.)
Around 6 months is a good time to prepare your baby for drinking from a cup. Start with water in a sipper cup and you will find it much easier to wean from the breast or bottle later. It’s important not to put your baby to bed with a bottle. Going to sleep with a bottle of milk or juice will start to cause tooth decay. If they want to suck on something to settle themselves, it’s better to use a pacifier/dummy.
Caring For Your Baby's Teeth | KidsHealth NZ has excellent advice on caring for your baby's teeth.
Returning to work outside the home
Breastfeeding
Many mothers go back to work and keep breastfeeding their babies. You can continue to breastfeed by:
- expressing breast milk so that someone else can feed your baby
- having your baby looked after near your work, so you can go and feed them
- having your baby with you at work
- having someone bring your baby to you at work for feeds.
Talk to your family and friends to see how they can help. Your midwife, Well Child Tamariki Ora nurse or doctor can give you advice.
By law, employers must give you unpaid breaks to breastfeed your baby or express milk at work, and must provide you with facilities to do this. If you are having problems getting this time, then someone at your work should be able to help you, or you can get advice from the websites below.
Useful websites
The Health New Zealand | Te Whatu Ora website has a useful section on Breastfeeding and returning to work - Health Information and Services Feeding » Whānau Āwhina Plunket is also very helpful.
The Breastfeeding Friendly Workplaces website has useful information about your right to breastfeed at work and advice on how to manage.
For more information on parental leave, go to Parental leave » Employment New Zealand
Childcare
Explore early childhood education services, kōhanga reo and other learning options near you. Research online, look in your newspaper, or ask other whānau members, parents and neighbours about their experiences. You can also search the Yellow Pages, contact 0800 ECE ECE, 0800 323 323 or contact your local Ministry of Education office. Check out the Ministry of Education’s website for Choosing an early learning service and the ERO report Early Childhood Education: A Guide for Parents | Education Review Office
Ask for help and support from your partner, family/whānau and friends. Discuss your support needs with your Lead Maternity Carer, Well Child Tamariki Ora nurse or doctor.
Babysitting – your sitter must be at least 14 years old
Anyone who looks after young children should learn first aid and rescue breathing. Talk to your Well Child Tamariki Ora nurse or doctor about where you can learn this.
See also First aid and CPR.
It is also important that you know that your sitter is safe with a crying baby. Make sure that they know what to do if your baby is unsettled.
Make sure your babysitter knows how to find your contact and emergency numbers.
Family violence and child abuse
Everyone in a family/whānau should feel safe and nurtured. Any behaviour by a family member that makes someone else feel controlled and fearful is never OK.
Family violence has a serious impact on children’s healthy development and behaviour, which can last their whole life.
Are You OK | Family Violence Information and Support has plenty of information, advice and resources, as well as links to various organisations that can help.
If you or your children feel unsafe in any way, you can talk to your Lead Maternity Carer, Well Child Tamariki Ora nurse or doctor. Someone in your family or whānau may also be able to help and there are community agencies who are there to support you.
You can also contact Oranga Tamariki Ministry for Children 0508 FAMILY, 0508 326 459 and talk to a social worker.
If you fear for your immediate safety, call 111 for help.
For more information, see Keeping your child healthy and safe
Stress, tiredness and frustration
Stress, tiredness and frustration can make it hard for parents and caregivers to deal calmly with a crying child, tantrums or challenging behaviour without losing their own control.
See also Coping with a crying baby
Your time together from 6 months to 12 months
Good to know
Helping your child learn and grow
- Enjoy time hugging, playing with, and reading to your child.
- Talk, sing and play music to your child.
- Give your child lots of tummy time awake on the floor to help them explore their world and develop their muscles.
Keeping your child healthy
- Breastfeeding is still the best for your child.
- If bottle feeding, hold your child while feeding and do not put them to bed with a bottle.
- Children are usually ready for and need extra food at around 6 months of age. Ask for the booklet Eating for Healthy Babies and Toddlers (HE1521). You could also see resources on infant feeding
- To protect against tooth decay, do not put sweet drinks in your child’s bottle.
- If using a dummy, do not dip it in sugar, honey or sweetened drinks, and do not let other children share it.
- Start brushing your child’s teeth twice a day with half a pea-sized amount of fluoride toothpaste as soon as the first tooth erupts, and particularly at night before bedtime.
- Enrol your child with the Community Oral Health Service for advice about looking after their teeth and preventing tooth decay, and for future regular dental care – it’s free.
Keeping your child safe
- Infant car seats should remain rear facing until your child is at least 2 years old.
- Keep nappy buckets and other water containers empty if you are not using them. To prevent drowning, cover them when they are full and keep them out of reach.
- Always watch your child in or near water.
- Know what your child can do physically and supervise them from an appropriate distance.
- Avoid small, hard foods (or small toys) because of choking risks. See Choking
- Keep household cleaners, dishwasher powder and chemicals out of reach to avoid poisoning and burns.
- Child-resistant lids help protect babies and children from poisoning.
- Have a smokefree and vape free home and car (see the Smokefree website).
- Never shake, hit or smack your child – if you feel you might lose control, put them in a safe place and walk away for a short time.
- Sleeping your child flat on their back – no pillow – and in their own bed helps protect against Sudden Unexpected Death in Infancy (SUDI).
Tō kōrua noho tahi mai i te 6 marama ki te 12 marama
He pai ki te mōhio
Te āwhina i tō tamaiti ki te ako me te tipu
- Me pārekareka ki te tākaro, te awhiawhi, me te pānui ki tō tamaiti.
- Kōrero, waiata me te whakatangi pūoro ki tō tamaiti.
- Me whai wā tō pēpi i a ia e oho ana ki runga i tōna puku ki te papa hei āwhina i a ia ki te hōpara i tōna ao me te whakawhanake i ōna uaua.
Te tiaki kia ora tō pēpi
- Ko te waiū te mea pai rawa mā tō tamaiti.
- Mēnā kei te whāngai mā te pātara, puritia tō tamaiti i te wā whāngai, ā, kaua e tuku ki te moe me tētahi pātara.
- Ko te tikanga kua pai ngā tamariki ki te whiwhi kai atu anō i te 6 marama. Me tono i te pukaiti Eating for Healthy Babies and Toddlers
- Hei ārai i te pirau niho, kaua rawa e whakakī i te pātara a tō tamaiti ki te waireka.
- Mēnā kei te whakamahi tami, kaua rawa e tautau ki te huka, mīere, waireka rānei, ka mutu kaua e tuari ki ētahi atu tamariki.
- Me tīmata te parāhe niho ina puta tonu mai te niho tuatahi o tō tamaiti kia rua ngā wā i te rā mā tētahi pani niho pūkōwhai, otirā i te pō i mua i te hokinga ki te moe.
- Whakaurua tō tamaiti ki te Ratonga Hapori Hauora Noho mō ngā tohutohu mō te tiaki i ōna niho me te ārai i te pirau niho, me ngā hauora niho o muri mai – kāore he utu.
Kia haumaru tō pēpi
- Me anga whakamuri ngā tūru waka kōhungahunga kia 2 tau rā anō te pakeke o tō tamaiti.
- Kaua rawa e waiho he wai ki roto i ngā pākete kope me ētahi atu ipu wai mēnā kāore ēnei i te whakamahia. Taupokina mēnā kei te kī me te waiho ki tētahi wāhi e kore e taea e te tamariki kia kore ai e toremi.
- Me mātakitaki koe i tō tamaiti i ngā wā katoa i a ia i roto, tūtata rānei ki te wai.
- Me mōhio koe ki te kaha ā-tinana o tō tamaiti, ā, ka whakahaere i a ia mai i tāhaki.
- Kaua ngā kai iti, mārō (taputapu tākaro iti rānei) kei raoa. Tirohia "Choking" i te whārangi 150 mō ētahi atu mōhiohio e pā ana ki te raoa i te kai.
- Waiho ngā matū horoi whare, paura horoi rīhi me ētahi atu matū ki tētahi wāhi e kore ai e taea hei ārai atu i te paihana me te wera.
- Ka tiaki ngā taupoki raka i ngā pēpi me ngā tamariki kia kore ai rātau e paihanatia.
- Kia auahi kore, rehutupeka kore hoki te kāinga me te waka (tirohia te
paetukutuku smokefree.org.nz). - Kaua rawa e rurerure, e patu, e papaki rānei i tō pēpi – mēnā ki tō whakaaro ka keka koe, me waiho te pēpi ki tētahi wāhi haumaru ka hīkoi atu mō tētahi wā poto.
Tirohia Kia haumaru, kia ora tō tamaiti
Having fun with your child from 6 to 12 months
Most of the best ‘toys’ for your baby at this age are in your home – for example, pots and pans or cardboard boxes. But your baby will learn best of all from the time you and other family/whānau spend with them.
Talk to your baby while you are dressing, bathing and feeding them, and make eye contact while you talk. When your baby makes sounds, repeat the sounds back so they learn to talk with you. They learn by hearing you – they will understand what you say before they start to talk. If you speak te reo or another language that is not English, your child will easily pick up both languages.
When you ask them to say the names of things they know, don’t expect them to say the word clearly!
Play simple games like peek-a-boo. Point out and name things that can be seen and heard. Sing and tell stories. Read books to your baby and describe the pictures.
Your child will enjoy nursery rhymes, waiata, hand games, etc.
For ideas for action games, ask your local library or early childhood centre and kōhanga reo. For resources on active play, see Sit Less, Move More, Sleep Well: Active play guidelines for under-fives resources | Ministry of Health NZ
Let them hear your own favourite stories, music, and rhymes.
Bedtime and other routines help make your baby feel secure. They might become attached to a toy or blanket they like to take to bed, to keep them company and to help them settle. From 9 months to 12 months, children learn by touching everything. This is normal, but you will need to keep dangerous and breakable things out of reach.
Praise them when they try to do things right, and ignore the behaviour you don’t like.
Sleeping
By 6 months some children may sleep through the night without a feed but many continue to wake at night until 12 months and older.
You can’t make a child sleep if they don’t want to. But you can encourage them to develop good sleep habits by having a regular bedtime with good routines, such as a bath and a story after dinner. Try to avoid busy play just before bedtime - make sure this is a quiet time. If you are worried about your baby’s sleeping, it may help to talk to your nurse or doctor or call Plunketline 0800 933 922
Try to keep to the safe sleep practices that you have been using with your baby. Continue to place them in their own baby bed (cot, bassinet), don’t use a pillow and place them flat on their backs – this keeps their airway clear for breathing.
Car seats and strollers should only be used for travelling and not as a sleeping device when you are at home or at your destination.
Safe sleep and SUDI
Sudden Unexpected Death in Infancy (SUDI) is a risk to babies until they are about 12 months old, but most SUDI is preventable. There are things we can do to protect our babies.
Although for some babies the cause of death is never found, most SUDI happens when a baby is sleeping in an unsafe way.
Babies may begin to roll over from their back to their front when they get to 5 or 6 months old. You don’t need to try and stop this from happening, as long as their cot is free of things that might suffocate them such as pillows, large soft toys or cot bumpers and there is no chance of them being caught between the mattress and the side of the cot.
Make every sleep a safe sleep
The safest place for all babies to sleep at night is in their own cot or bassinet, close to parents/caregivers and in the same room.
Always follow these safe-sleep routines for your baby and your baby’s bed:
- Make sure your baby is in their own bed for every sleep (and in the same room as parents/caregivers at night).
- Make sure your baby is on their back for every sleep.
- Keep your baby smokefree and vape free from the start (including in the car).
- Breastfeed your baby.
- Immunise your baby on time.
- Make sure your baby's bed is free of things that might suffocate them such as pillows, large soft toys or cot bumpers.
If you are out somewhere, or if you are sleeping with your baby, make sure they have their own safe place to sleep. If you go out, remember to take your portacot with you.
It is never safe to put your baby to sleep in an adult bed, on a couch or on a chair.
Car seats or capsules protect your baby when travelling in the car. Don’t use them as a baby bed at home or at your destination.
If you don’t have a baby bed, ask your Lead Maternity Carer or child health nurse. If you are on a low income, you may be able to receive a Special Needs Grant from Work and Income to buy a bed.
For more information visit Work and Income or call 0800 559 009.
Make sure your baby’s bed is safe
Your baby’s bed needs a firm flat mattress that fits snugly so your baby can’t get into any gaps between the frame and the mattress. There should be nothing in the bed that could cover their face or lift their head – no toys, pillows, loose bedding or bumper pads. Babies don’t need pillows and are safest sleeping flat on their backs.
There are choking and strangling risks in the bedroom too. Make sure that cots are assembled correctly. The tops on the corner posts of wooden cots may need to be sawn off so your child can’t hang themselves by their clothing. Consumer Affairs New Zealand states that spaces between the bars of the cot must be between 50 mm and 95 mm. Try to make the spaces closer to 50 mm if you can.
The cords for blinds and curtains are a danger. Put the cot away from the window so your child can’t reach them.
For more on preventing choking and strangling, see Choking, strangling, suffocating.
Make sure your baby is healthy and strong
It is important to keep your home and car smokefree and make sure that others don’t smoke or vape around the baby. This will help your baby grow strong and healthy.
Keep breastfeeding your baby for the first year, and beyond if you like. Make sure your baby is immunised on time.
For more on safe sleep, see Protecting your baby from SUDI
If you find your baby not breathing, call for help, and begin rescue breathing (CPR) immediately.
Feeding your baby
Keep feeding your child breast milk until they are at least 12 months old. If this is not possible, the only suitable alternative for children under 12 months is a specially formulated breast milk substitute (infant formula). Some mothers continue breastfeeding past this time. It’s up to you and your child to decide when is the time to stop. Start giving some solids when your child is ready and needs extra food – this will be at around 6 months of age.
Your child may be ready to start solids if they:
- are around 6 months of age
- can hold their head up and sit with less help
- open their mouth as food approaches
- can keep food in their mouth and then swallow it, instead of pushing the food out.
Ask for the flyer Starting Solids (HE6014) and the booklet Eating for Healthy Babies and Toddlers (HE1521). You could also see Te Whatu Ora | Health Promotion's resources on infant feeding.
Give the milk feed first and offer solids as a ‘top up’ – e.g., try 1 teaspoon first and slowly add more until your child is having about 3–4 teaspoons at a meal. First foods need to be plain, smooth and soft, such as:
- cooked and puréed (smooth with no lumps) lean lamb, beef, chicken, or puréed lentils and beans
- iron-fortified baby rice or infant cereal
- puréed kūmara, kamokamo, pumpkin, potato, carrot or marrow
- puréed apple, pear, apricot, peach, ripe mashed banana or avocado.
From 7 months, you can introduce more texture by giving mashed rather than puréed vegetables and fruits. By 8 months some children are ready to try finger food in pieces that they can easily pick up and put in their mouths. Try pieces of very soft vegetables and fruit (e.g., ripe banana, well-cooked pumpkin), toast fingers and thin slices of cheese.
Babies do not need added sugar or salt.
Vegetarian babies can get iron from cooked dried beans and legumes, tofu, green leafy vegetables, egg yolk, wholemeal cereals and breads, and iron-fortified cereals. Vitamin C found in fruits and vegetables improves iron uptake from a vegetarian diet when eaten at meals. If you are bringing up your baby as a vegetarian or vegan, it is important that you get dietary advice, as babies need a different nutritional balance from an adult.
By 8 or 9 months, you can give solids before their milk feeds.
Why solids shouldn’t be started too late
To grow and learn well, your baby needs the vitamins and minerals (especially iron) in solid foods from around 6 months of age. The nutrients in solid food help your baby’s brain and body to develop. If you would like to know more about healthy eating for your child, or if you are worried about how your child is growing, talk to your Well Child Tamariki Ora nurse or doctor.
A child is not always hungry. Getting upset about them refusing food makes it worse. It could just be time to offer smaller helpings or a new food.
Choking
Babies and young children can choke easily, so feed them only when they are seated and always stay with them while they eat.
Be aware of some high-risk foods, such as small hard foods (like nuts, raw carrot or apple); small round foods (for example, grapes, raisins or watermelon seeds); skins or leaves (for example, stone fruits, lettuce); compressible foods (like hot dogs, pieces of cooked meat); thick pastes (e.g., chocolate spreads, peanut butter); and fibrous or stringy foods (for example, celery).
To avoid choking:
- alter the food texture if necessary – you can grate, cook, finely chop or mash the food
- remove the high-risk parts of the food, for example, peel the skin or remove strong fibres, pips and seeds from fruit and vegetables
- do not give small, hard foods such as whole nuts and large seeds until children are at least 5 years old.
For more information on food-related choking, see Higher choking risk foods for children under 5
Supporting healthy eating habits early in life
Parent and whānau - Role modelling
Young children will copy what their caregivers, siblings and whānau do, so it helps if the family eats the same healthy foods that you offer your baby or toddler.
Your role is to decide what food to offer your baby or toddler. Your baby or toddler decides how much they want to eat.
Hungry or full
Babies and toddlers are good at knowing when they are hungry and when they have had enough to eat. It’s important you feed your baby and toddler when they are hungry and stop feeding them when they have had enough to eat.
Having a mealtime routine is important as it gives your baby or toddler regular opportunities to eat.
Signs your baby or toddler may be hungry:
- puts their hands in or near their mouth
- is more active, moving their hands and feet
- reaches for or points to food
- opens mouth when offered a spoon or food
- cries – crying is usually a late sign of hunger in babies
It is also important to stop feeding your baby or toddler when they are showing signs they have had enough to eat.
Signs that your baby or toddler is full:
- turning head away
- pushing food away or arching away
- sealing lips
- spitting out food
- cries
Note: If you are worried that your baby isn’t getting enough to eat, or isn’t growing well, the best thing to do is contact your doctor or wellchild nurse.
Tips for mealtimes:
- Eat as a family where possible
- Eat what you want your child to eat
- Encourage your child to eat and praise desired behaviour
- Do not force your child to eat. If your baby is showing signs of fullness, you should stop feeding, even if the baby has eaten less than usual or less than you would like them to eat.
- Only offer food because a child is hungry and not for other reasons, entertainment, reward or to control behaviour.
- From a young age, encourage your child to feed themselves.
- Limit access to foods with added sugar and salt.
Looking after baby teeth
Your child may have some teeth by now.
Look after ‘baby’ teeth. Sweetened drinks, foods and fruit juices can cause tooth decay (holes) and cause your child to develop a taste for sweetened foods. Avoid putting your child to bed with a bottle, as the milk, formula or juice can harm their teeth as they sleep.
Baby teeth are important in helping your child to eat and speak properly. Baby teeth also hold the space for adult teeth. They guide the adult teeth into their correct position and are important for the proper growth of the face and jaw.
As soon as teeth appear, you should start the habit of gentle brushing with a small, soft toothbrush and half a pea-sized amount of regular-strength fluoride toothpaste twice a day. One of these brushings should be last thing at night before bed.
Gently lift your child’s top lip once a month to check inside their mouth. It’s a quick and easy way to see whether decay is present in its early, treatable stages.
The NZ Dental Association has information on caring for infant and toddler teeth, including pictures at New Zealand Dental Association | Common Dental Problems (nzda.org.nz)
Look for chalky, white spots or patches at the gumline, particularly on the upper front teeth. Also look for discoloured areas or if any parts of the teeth are missing. Check that gums look healthy, not swollen or bleeding.
Discuss any concerns with your Well Child Tamariki Ora nurse at the next visit, or with your doctor, or contact your Community Oral Health Service – 0800 TALK TEETH, 0800 825 583
Make sure you enrol your child with the Community Oral Health Service. The service is free. It encourages children to be enrolled at birth so that parents/caregivers and family/whānau can actively participate in their child’s oral health care and learn to care for their child’s teeth at home. It focuses on preventing ill-health and intervening early if an examination finds tooth decay.
Once your child is enrolled with a Dental or Oral Health Therapist, it is important to keep appointments, including regular dental check-ups, even if you find no visible decay when you lift your child’s lip every month. Regular dental check-ups increase the chances that therapists will detect any signs of oral disease such as tooth decay early, which allows for timely treatment or preventive measures.
Useful websites
Health New Zealand | Te Whatu Ora website has a page on oral health at Caring for your child's first teeth as well as links to other websites.
The NZ Dental Association has excellent advice available at New Zealand Dental Association | Infants & Toddlers (nzda.org.nz)
Family/whānau relationships
Keep in contact with friends and family/whānau. Good family relationships are important for everyone. Strong family bonds are important for a baby’s brain development and emotional well-being.
Accepting help and support from family/whānau helps everyone be involved, and will make things easier for you too (see Looking after yourself).
Take some time to be with your partner and with your other children.
It is good for partners to be involved in some child and health care too (see Partners are needed too). Other children will want to be involved as well.
Your child between 1 and 2 years
Good to know
Helping your child learn and grow
- Give your child lots of hugs and praise.
- Listen and talk to them – notice them when they are good.
- Don’t expect too much of them.
- Read, sing, tell stories and play together, rather than use a screen.
- Show your child you are physically active, and they will learn from you – walking to the park, playing with a ball, etc.
Keeping your child healthy
- Toddlers need three small meals a day and small healthy snacks in between – they have small stomachs and lots of energy.
- Brush your child’s teeth twice a day with half a pea-sized amount of fluoride toothpaste.
- If your child uses a dummy, try to stop using it by the time they are 2 years old.
- Never put anything sweet, like honey, on a dummy.
- If your baby has been bottle feeding, avoid using a bottle after they are 12 months old.
- Avoid putting your child to bed with a bottle.
- From 6 months of age, you can introduce a cup.
- Your child will need help and supervision as they learn to hold the cup with two hands and bring it up to their mouth themselves.
- Choose foods and drinks low in sugar to reduce the risk of tooth decay.
- Water or full-fat cow’s milk are the best drinks for your child.
- Children do not need sugary or salty foods.
- Lift your child’s upper lip every month to check for signs of tooth decay.
- Make sure your child is enrolled with the Community Oral Health Service.
- Immunisation (due at 12 and 15 months) helps protect your child from serious infectious diseases.
Keeping your child safe
- Use a child car seat in all cars, for all trips.
- Offer safe places to crawl, walk, run, jump and climb.
- Have fenced areas for outside play so that children can’t get on the driveway, the road or in water.
- Always watch your toddler in or near water.
- Know what your child can do physically, and supervise from an appropriate distance.
- Vertical bars on fences make it hard for children to climb over to dangers.
- Only offer toddlers and young children food when they are seated, and stay with them while they eat.
- Show your child you are physically active, and they will learn from you - walking to the park, playing with a ball, etc.
- Toddlers and young children can choke easily. Don’t give them hard foods, such as nuts or small hard sweets.
- Ask your pharmacist for child-resistant caps on all medicines and store them out of reach.
- Talk to your childcare centre about how they will keep your child safe.
- Keep lighters, matches and candles out of reach.
- Have a smokefree and vape free home and car.
- Never shake, hit or smack your toddler – if you feel you might lose control, put them in a safe place and walk away for a short time.
Looking after yourself
- See and talk to friends, family, whānau.
- Join playgroups, parent groups.
Ko tō tamaiti i waenganui i te 1 me te 2 tau
He pai ki te mōhio
Te āwhina i tō tamaiti kia ako me te tipu
- Kia nui te awhiawhi me te whakanui i tō tamaiti.
- Whakarongo me te kōrero ki a ia – me aro ki a ia ina pai ia.
- Kaua e tino nui rawa ō tūmanako mōna.
- Pānui, waiata, kōrero pūrakau me te tākaro tahi ki a ia, kaua te pouaka whakaata me te kōpae ataata anake.
Te tiaki kia ora tō tamaiti
- Kia toru ngā kai iti mā ngā kōhungahunga ia rā me ngā paramanawa tōtika i waenga – he iti ō rātau puku, he nui te toritori.
- Parāhehia ngā niho o tō tamaiti kia rua ngā wā i te rā mā te pani pūkōwhai.
- Mēnā he whakamahi tami tō tamaiti, me whakamutu i mua i te ekenga ki te 2 tau.
- Kaua rawa he whakareka pēnei i te mīere ki te tami.
- Mēnā kei te whāngai koe i tō pēpi mā te pātara, me whakamutu te whakamahi pātara i muri o te 12 marama.
- Mai i te ono marama te pakeke, ka taea te hoatu kapu.
- Me āwhina, me tirotiro i tō tamaiti i a ia e ako ana ki te pupuri i te kapu me ngā ringa e rua, me te hiki i te kapu ki tōna waha.
- Me whāngai ki ngā kai me ngā inu he iti te huka hei whakaiti i te tūponotanga ki te pirau niho.
- Ko te wai, te miraka whai mōmona a te kau rānei ngā inu pai rawa mā tō tamaiti.
- Ki te whāngaihia e koe tō tamaiti ki ngā kai whai huka, ko ngā wā kai te wā pai kaua hei paramanawa ka mutu me iti noa ngā wā (iti ake i te kotahi i te wiki).
- Hei aha te huka i ngā kai mā ngā tamariki.
- Hikina te ngutu o runga o tō tamaiti ia marama ki te tirotiro mō ngā tohu tuatahi o te pirau niho.
- Me whakarite kua whakaurua tō tamaiti ki te Ratonga Hapori Hauora Noho
- Ka āwhina te ārainga mate (hei te 15 marama) ki te tiaki i tō tamaiti mai i ngā mate hōrapa taumaha.
Kia haumaru tō tamaiti
- Whakamahia he tūru waka tamariki ki roto i ngā waka katoa, mō ngā haerenga katoa.
- Me tuku wā ngōki, hīkoi, omaoma, pekepeke me te pikipiki haumaru.
- Me tākaro i waho i roto i ngā wāhi taiepa kia kore ai e eke ki runga i te ara kuhunga, huarahi, te wai rānei.
- Me mātakitaki koe i tō tamaiti i ngā wā katoa i a ia i roto, tūtata rānei ki te wai.
- Me mōhio koe ki te kaha ā-tinana o tō tamaiti, ā, ka whakahaere i a ia mai i tāhaki.
- He uaua mō ngā tamariki te piki i ngā pae torotika i runga taiepa ki ngā wāhi mōrearea.
- Me hoatu anake i te kai ki ngā kōhungahunga me ngā tamariki paku i te wā e noho ana rātau, ā, me noho tonu i tō rātau taha i a rātau e kai ana.
- Ka raoa noa iho ngā kōhungahunga me ngā tamariki paku. Kaua rawa e whāngai ki ngā kai mārō pēnei i ngā nati, ngā rare iti mārō rānei.
- Me pātai koe ki tō taka rongoā mō ngā taupoki raka mō ngā rongoā katoa ka waiho ki tētahi wāhi e kore e taea e te tamariki.
- Me kōrero koe ki tō pokapū tiaki tamariki ka pēhea tā rātau tiaki i tō tamaiti kia haumaru ia.
- Me waiho ngā whakakā, hika ahi me ngā kānara kia kore ai e taea e te tamariki.
- Kia auahi kore, rehutupeka kore hoki te kāinga me te waka.
- Kaua rawa e rurerure, e patu, e papaki rānei i tō kōhungahunga – mēnā ki tō whakaaro ka keka koe, me waiho ia ki tētahi wāhi haumaru ka hīkoi atu mō tētahi wā poto.
Tirohia Kia haumaru, kia ora tō tamaiti
Te tiaki i a koe anō
- Kōrero ki tō whānau, ō hoa, kiritata hoko.
- Whakauru atu ki ngā rōpū tākaro, rōpū mātua.
Having fun with a toddler
Children learn by trying to do things themselves when they play. They like to be busy. You can help by:
- letting them make a mess and have fun using water, sand, clay, pot cupboards
- giving them interesting things to play with – play dough, textured fabrics, leaves
- giving them ideas for new things to try and do – pasting, drawing, building
- being pleased when they learn any new skill
- talking, reading and singing together
- letting your toddler be with other children
- encouraging make-believe play, providing dress-up gear
- showing your child how to use a runner/balance bike.
For more ideas, ask at your local library, early childhood centre and kōhanga reo.
There is also a link between learning and movement. The Ministry of Health has published Guidelines for active play for under fives
Speech and language development
Talk to your child – about what they are doing and what is happening around you during the day. Use short, simple sentences and praise their attempts to talk to you. If they say a simple word, build on it – for example, if your child says 'Ball', you could say, 'That’s a red ball, roll the ball'. Look at books together, tell the story and describe the pictures.
Toddler discovering ‘me’ – good ways to get what you both want
As a baby grows into a toddler, they begin to find out who ‘me’ is.
Notice them when they are good. Praise makes them want to do the things that please you.
They like to make simple choices, like which shirt or shoes to wear.
‘No’ becomes a favourite word. Ask questions that cannot be answered with ‘no’.
Children learn a lot by watching you. If you are kind and loving with a child, even when you have to be firm, it will help them learn self-control from you.
When you listen to children, they know you care about how they feel. Don’t expect too much of them. Toddlers are still learning to understand how you want them to behave.
If there is a new baby, spend some special time alone with your toddler. Make them feel proud of being old enough to help with care of the new baby.
Feeding fun
Toddlers can have small amounts of the same food that you and your family/whānau eat, along with about 350 ml of milk each day. You will still need to take care with food texture to prevent choking. Do not give small, hard foods such as whole nuts and large seeds until children are at least 5 years old.
Don’t worry if your toddler seems to be a ‘fussy’ eater. Most children will eat when they’re hungry, although they may eat very little at times. As long as they are growing well and have lots of energy, just keep offering healthy choices. Don’t worry if they refuse some things – they’ll make up for it by eating other foods. For example, they may reject some vegetables but gobble up plenty of fruit instead. Offer smaller helpings if they reject food and offer the rejected food later on.
Avoid giving fatty or fried foods, or foods high in sugar or salt. Children who eat ‘treat’ foods too often tend to want less healthy food.
Tips for fussy eating
Toddlers like to be independent and will let you know what they do and don’t like. Some will drink and eat everything they’re offered, while others pick and choose.
They may suddenly refuse a food that was a favourite. Even the best eaters are fussy at times. Here are some tips that may help.
- Offer small amounts of the foods they refuse along with foods they like.
- Try to serve meals before your child is tired, or have your evening meal earlier. Offer a variety of foods during the day, as a tired child may not eat well at night.
- Keep offering small amounts of new foods, especially vegetables and fruits. Children often learn to enjoy different foods even when they refuse them at first.
Try not to battle over mealtimes. Give them a range of healthy foods and let them choose what they want and how much. Don’t bribe, force or nag over leftover food – it’s better to praise them for trying.
Present your child’s food in different ways – for example, offer meat as hamburgers or meatballs. Involve your child in preparing food, as this may increase their interest.
Offer your child simple choices – e.g., ‘Do you want an apple or banana?’ This will help them feel they have some control.
Avoid snacks just before meals. A 1 to 2 hour gap will help them feel hungrier by meal time. If your child asks for food but doesn’t seem hungry, try to keep them busy.
It’s best to offer drinks in a cup rather than a bottle. Check how much they are drinking, as too much milk can reduce their appetite. Toddlers can usually have up to 350 ml of milk per day.
Eat together sitting down as a family and remove other distractions (like the TV). Eat the foods you want your children to eat. They love to copy what you do.
If your toddler is refusing food for longer than 2 weeks reach out to your GP or
follow the questionnaire at Feeding Matters - Serving Kids with Pediatric Feeding Disorder
Food for energy and growth
Children eat small amounts, and so they need three small meals a day and small healthy snacks between meals, such as:
- crackers and little sandwiches
- pieces of soft or grated raw or cooked cold vegetables and/or fruit
- breakfast cereals – choose cereals that are low in sugar
- yoghurt, milk, or small, thin slices of cheese
- soft, slightly mashed, cooked dried peas, beans or lentils
- chopped hard-boiled egg, finely chopped pieces of soft lean meat or chicken
- pasta or rice-based meals.
Remember to cut food to a size your child can easily hold and eat, and offer food that matches your child’s ability to chew and grind. Most young children can’t grind hard food until they get their final molars, which is usually between 2½ and 3 years of age.
See Choking for what to do if your child is choking.
Children need to be offered plenty to drink – more when they are busy and when it’s hot. If your child is thirsty, water is the best drink.
Fruit drinks, juice, flavoured milk and fizzy drinks are high in sugar and are harmful for children’s teeth. It’s best to choose either water or plain milk and keep other drinks for treats. Infants and toddlers do not need juice, cordials, fruit drink, flavoured milk, soft drinks, tea, coffee or alcohol to drink.
Teeth – time to teach brushing twice a day
Help your child with the habit of brushing their teeth twice a day – after breakfast and before bed. If you start cleaning your child’s teeth as soon as they come through, toothbrushing becomes a routine and your child will allow you to help them. Children need help to clean their teeth until they are around 8 or 9 years old.
Use a small toothbrush with soft bristles and half a pea-sized amount of regular-strength fluoride toothpaste to help harden and protect the teeth. You may find it easier to stand behind your child and gently tilt their head back as you brush. Brush all around the inside surfaces, where teeth meet the gums, and also the top chewing surfaces. On the front of the teeth, brush in tiny circles all around the outside surfaces, close to the gums.
Don’t rinse the mouth with water, but teach children to spit out the left-over toothpaste. By not rinsing toothpaste from the mouth after brushing, fluoride remains in contact with the teeth for longer and can more effectively prevent tooth decay.
Toothpaste should not be eaten and children should be supervised when they use toothpaste.
As your child gets older, it’s a good idea to let them try using their toothbrush after you have cleaned their teeth for them. Most toddlers and young children enjoy doing this.
Make sure you look after your own teeth well – your child will learn most about how to clean their teeth by copying you. Also, your child can catch bacteria from you that cause tooth decay – for example, if you share spoons or your toothbrush.
If you haven’t been contacted by the Community Oral Health Service yet, check to make sure you are enrolled, or to or get an appointment – phone 0800 TALK TEETH, 0800 825 583
It is important to keep appointments, including regular dental check-ups, even if you find no visible decay when you lift your child’s lip every month. Regular dental check-ups increase the chances of finding and treating any tooth decay early.
If your child accidentally bumps their teeth, it is important that you take them to a dental therapist or oral health therapist in the Community Oral Health Service, even if the teeth still look all right. The oral health professional can check that no damage has been done to the nerves or to the developing teeth.
Useful websites
The Health New Zealand | Te Whatu Ora website has a page on Caring for your child's first teeth including links to other websites.
HealthEd includes resources such as Caring for Teeth (HE1524) and It's Easy to Protect your Family's Smile (HE2248)
New Zealand Dental Association | Infants & Toddlers (nzda.org.nz) has excellent advice
Caring For Your Child's Teeth: 1 To 5 Years | KidsHealth NZ
Having fun with a toddler
Your toddler is learning about their body and trying to do a lot of new things. However, they can’t see danger and so rely on adults to keep them safe. They are more likely to be injured between 1 and 2 years of age than at any other time in their life. It is really important to make sure that someone is keeping an eye on your toddler at all times. This is especially important when there are lots of people around, or if you are in an unfamiliar place.
For ideas and information on safe activity, see the Sport New Zealand website.
See also Keeping your child healthy and safe
Toilet training
A child will be ready to start learning to use the toilet any time between about 20 months and about 3 years. Every child learns at a different pace.
The right time will be when they:
- know when they are wet or dirty
- are beginning to try to do things without your help.
Teach your child to wash their hands each time after using the toilet.
Information on toilet training can also be found at Toilet Training | KidsHealth New Zealand's Trusted Voice On Children's Health
Your child between 2 and 3 years
Good to know
Helping your child learn and grow
- Spend time with your child, listen and talk to them. This grows the bond between you, helps them feel loved and secure, and helps their language development.
- Use words for feelings, both yours and theirs (e.g., happy, sad, angry).
- Notice when they are good and praise them.
- Read to them every day – limit time spent with screens, or electronic games to less than 1 hour a day.
- Play with your child inside and outside. Find safe places to crawl, walk, run, jump and climb.
- Show your child how to use a runner/balance bike.
- Show your child you are physically active, and they will learn from you - walking to the park, riding your bike, playing with a ball, etc.
Keeping your child healthy
- Young children need lots of small meals and healthy snacks. Home prepared food for your baby or toddler does not need salt or sugar added.
- If using commercially-prepared foods, choose those that are low in salt (sodium) and with no added sugars.
- Choose nutritious and tooth-friendly snacks.
- Water and milk are best to drink.
- Brush your child’s teeth twice a day with half a pea-sized amount of regular-strength fluoride toothpaste. Your child needs your help to brush their teeth until they are 8 or 9 years old.
- Lift the lip once a month to check for signs of tooth decay – ask your Well Child Tamariki Ora nurse to show you how to do this.
- Make sure your child is enrolled for and attends regular visits at the Community Oral Health Service 0800 TALK TEETH, 0800 825 583
Keeping your child safe
- Children can move quickly and need to be kept an eye on at all times, especially when there are lots of people around or they are in unfamiliar places.
- Fenced areas for outside play help to stop children getting on the driveway or road.
- Always hold your child’s hand to cross the road.
- Know what your child can do physically, and supervise from an appropriate distance.
- Helmets and shoes protect heads and feet on trikes.
- Use a child car seat in all cars, for all trips.
- Children will copy you so make sure you keep lighters, matches and candles where children can’t reach them.
- Have a smokefree and vape free home and car and don't keep lighters and matches in the car.
- Never shake, hit or smack your child. If you feel you might lose control, put them in a safe place and walk away for a short time. See Behaving well
Ko tō tamaiti i waenganui i te 2 me te 3 tau
He pai ki te mōhio
Te āwhina i tō tamaiti ki te tipu me te ako
- Me whai wā koe ki te whakarongo me te kōrero ki a ia. Ka tipu te hono ki waenga i a kōrua, ka rongo ia i te aroha me te manaaki, ā, ka āwhina ki te whakapakari i tōna reo.
- Whakamahia ngā kupu kare ā-roto, āu me āna (hei tauira, harikoa, pōuri, riri).
- Me aro atu ina pai ia me te whakanui i a ia.
- Me pānui ki a ia ia rā – kia iti ake i te rua haora i te rā te wā ka whakapaua ki te pouaka whakaata, kōpae ataata, me ngā tākaro ataata.
- Me tākaro koe me tō tamaiti ki rō whare me waho. Kimihia ngā wāhi haumaru ki te ngōki, hīkoi, omaoma, pekepeke me te pikipiki.
Te tiaki kia ora tō tamaiti
- Kia nui tonu ngā kai iti me ngā paramanawa hauora mā ngā tamariki paku. Waiho ngā kotakota rīwai, pihikete reka, aha atu aha atu mō ngā wā hari. Hei aha te tote me te huka i ngā kai ka whakatakahia mā tō pēpi, kōhungahunga rānei i te kāinga.
- Mēnā e kai ana i ngā kai whakataka ā-arumoni, kōwhiria ngā kai e iti ana te tote, ā, kāore he huka i tāpiritia.
- Me whiriwhiri ko ngā paramanawa whai painga, pai hoki mō ngā niho.
- Me whiriwhiri ko ngā kai me ngā inu iti te huka.
- Ko te wai me te miraka ngā inu pai rawa.
- Parāhehia ngā niho o tō tamaiti kia rua ngā wā i te rā mā te pani pūkōwhai. Me āwhina koe i tō tamaiti ki te parāhe i ōna niho kia eke rā anō tōna pakeke ki te 8, ki te 9 tau rānei.
- Hikina te ngutu o runga kia kitea ngā tohu tuatahi o te pirau niho – pātai atu ki tō kaiwhakarato Tamariki Ora me pēhea te mahi i tēnei.
- Me whakauru e koe tō tamaiti ki te Ratonga Hapori Hauora Niho 0800 825 583 ā, kia rite tonu ana toronga.
Kia haumaru tō tamaiti
- Ka taea e ngā tamariki te nekeneke wawe haere, ā, kia mātakitakina rātau i ngā wā katoa, otirā i te wā e maha ana te tangata, i ngā wāhi tauhou rānei.
- Ka āwhina ngā wāhi taiepa ki te ārai i te tamariki kia kore ai e puta ki te ara kuhuna, te huarahi rānei.
- Puritia te ringa o tō tamaiti ki te whakawhiti i te huarahi i ngā wā katoa.
- Me mōhio koe ki te kaha ā-tinana o tō tamaiti, me mātakitaki mai i tāhaki.
- He ārai wharanga ngā pōtae mārō me ngā hū i runga pahikara toru wīra.
- Whakamahia he tūru waka tamariki ki roto i ngā waka katoa, mō ngā haerenga katoa.
- Ka whai ō tamariki i a koe, nā reira me waiho ngā whakakā, ngā hika ahi me ngā kānara kia kore ai e taea e te tamariki.
- Mēnā e kai ana i ngā kai whakataka ā-arumoni, kōwhiria ngā kai e iti ana te tote, ā, kāore he huka i tāpiritia.
- Kaua rawa e rurerure, e patu, e papaki rānei i tō tamaiti – mēnā ki tō whakaaro ka keka koe, me waiho te tamaiti ki tētahi wāhi haumaru ka hīkoi atu mō tētahi wā poto. (Tirohia te whārangi 166).
Tirohia Kia haumaru, kia ora tō tamaiti
Having fun and learning
Your child will enjoy going to a playgroup or other early childhood group.
Dreaming, pretending and talking to themselves are important parts of your child’s play.
Your local library, early childhood centre and kōhanga reo will have more ideas and information about play. They may also have special toddler reading sessions. These are fun for your child – and for you.
There is also a link between learning and movement. Encourage your child to extend themselves in a safe way, by balancing, jumping, etc. Be a positive role model by being active – walking the dog, swimming, running, going for family walks.
There is also a link between learning and movement. The Ministry of Health has published Guidelines for active play for under fives
Speech and language development
Have simple conversations with your child. Follow their lead and talk about activities they are doing. Get their attention before you speak and reduce background noise and distractions.
When you talk to your child, use the same level of words and sentences that they do, or a little higher. Use positive language rather than negative – for example, 'Put the book on the shelf' rather than 'Don’t put your shoe on the chair' – and be specific – 'Put your cup on the table' rather than 'Put it there'.
Create the need to talk. Wait for your child to tell you what they want or need, or offer them two options when you ask them a question – 'Would you like to drink milk or water?' Give them time to think about it and reply. Reward their attempts to talk. Read books together and ask your child about the pictures – for example, 'Is the boy happy or sad?'
Behaving well
Helping children learn to behave the way you want them to is one of the toughest jobs of parenting. Copying you is one of the most important ways they learn. If you behave the way you want them to behave, they will learn from you.
Ignore unwanted behaviour or distract the child with something else. Unwanted behaviour may be a way of getting your attention. Listen to your child when they talk to you and spend time with them.
Get agreement and support from partners, family, whānau and other caregivers on screen time, eating, playing, bedtime and general expectations.
Children won’t stop loving you if you’re firm with them. They’ll feel a lot safer when they know what the limits are, even though they will test them sometimes. Being fair and consistent makes things easier for them – and for you.
For positive parenting ideas and courses, see Strengthening Families
Tantrums are normal – some ideas you might like to try
Try to avoid tantrums:
- give them time to say what they want or feel
- recognise the situations where your child is likely to have a tantrum, e.g., when they are tired, hungry or frustrated – have food and drink on hand or offer a distraction if you see the warning signs
- tell them what you would like them to do and be pleased if they do it.
If a child has a tantrum:
- ignore the tantrum and walk away a short distance until things have calmed down
- gently take them to a safe place for ‘time out’. (‘Time out’ means 2 to 3 minutes in a safe place away from contact with other people until things calm down.)
If a child’s behaviour is making you feel really angry and upset
Never shake, hit or smack your child. Put them in a safe place, like a bedroom (bathrooms or laundries can be unsafe places) and walk away from them until things cool down.
Call someone you trust if you feel you might lose control. Remember that words can hurt too.
Other sources of help
Your health district may run parenting courses and may provide counselling or therapy for you and/or your child if that is required. Your doctor or Well Child Tamariki Ora nurse will need to make a referral for you.
Phone PlunketLine 0800 933 922 or Healthline 0800 611 116. Young parents can phone Youthline on 0800 376 633
You can also find helpful information on the KidsHealth website.
Barnardos Aotearoa (phone 0800 BARNARDOS 0800 227 627 or 0800 KIDSTART 0800 543 782) also offer family support and counselling.
Caring for teeth
As your child gets older, it’s a good idea to let them try using their toothbrush after you have cleaned their teeth for them. Most toddlers and young children enjoy doing this, and your child may want to brush their own teeth by now. However, children cannot brush properly by themselves until they can control a pencil and begin to write. You should keep helping your child brush their teeth until they are 8 or 9 years old.
Teeth should be brushed twice a day with half a pea-sized amount of regular-strength fluoride toothpaste after breakfast and before bed.
You will need to put the toothpaste on the brush (half a pea-sized amount for children under 6) because small children will nearly always put too much on. Using too much toothpaste can mean your child’s fluoride intake is too high, and may affect adult teeth as they are forming in the gum, causing white speckles. Encourage your child to spit out the toothpaste after brushing and not to rinse with water. Make sure they do not eat toothpaste.
Make sure your child is enrolled with the Community Oral Health Service or a dentist and that you, other family members or whānau accompany them to appointments. Regular dental visits are vital for advice on keeping your child’s teeth healthy and to recognise and treat problems early.
If your child accidentally bumps their teeth it is important that you take them to a dental or oral health therapist in the Community Oral Health Service, even when the teeth still look all right. The oral health professional can check that no damage has been done to the nerves or to the developing teeth.
Bedtime
Children need their sleep – and so do you. You can decide to be firm about having a regular bedtime. Establishing a daily bedtime routine with cuddles and a story or a special toy will help make bedtime easier. Try to avoid busy play just before bedtime – make sure this is a quiet time. Talk to your child about how staying in bed after the light is out is a good thing to do. Praise them in the morning if they do it.
If your child gets out of bed, don’t react. Just put them back to bed. The idea is for them to get bored with the behaviour rather than you getting angry.
If you are having trouble with bedtimes, ask your Well Child Tamariki Ora nurse or doctor for advice or call PlunketLine 0800 933 922 to talk to a Well Child nurse.
See Normal Sleep | KidsHealth NZ for information on baby sleep and settling
Toilet training
When a child has been dry for a while in the daytime, they will usually start having some dry nights as well. This is a sign that you can start to talk about moving from a nappy or pull-ups to wearing pyjama pants at night. They will still have a few accidents, so be prepared to support and encourage them as they learn to be dry. It takes a lot longer for children to learn control at night than in the daytime, but some will learn quickly. Don’t push it at this age – wait until they are ready.
Sometimes children who are dry at night start wetting again. This can be due to stress (such as the arrival of a new baby or moving house), but will settle down quickly with positive encouragement and support. If it persists or you have concerns about it, ask your Well Child Tamariki Ora nurse or doctor for advice or call PlunketLine 0800 933 922
Don’t punish your child for ‘accidents’ – they are still learning. Reward them for getting it right.
Your child between 3 and 5 years
Good to know
Helping your child learn and grow
- Your child will enjoy time to play and friends to play with.
- Let them know they are special – tell them they are great.
- Notice when they are good and praise them.
- Listen to them tell you how they feel – spend time talking together.
- Have meal and snack times together.
- Spend individual time with each child.
- Read to them every day. Limit time spent with screens and electronic games to less than 1 hour a day.
Keeping your child healthy
- Children need many different foods from the four food groups every day:
- vegetables and fruit
- breads and cereals
- lean meats, chicken, seafood, eggs, dried beans, peas and lentils
- milk and milk products like cheese and yoghurt.
- Some children need more food than others.
- Offer healthy and tooth-friendly snacks and drinks and foods low in sugar to reduce the risk of tooth decay.
- Fruit drinks and juice, cordials and other sweetened drinks (including soft drinks and sports drinks) are not recommended.
- Brush your child’s teeth twice a day with just half a pea-sized amount of fluoride toothpaste.
- Lift your child’s lip once a month to check for signs of tooth decay.
- Continue to take your child for their regular dental check-up appointment or for any treatment that is required.
Keeping your child safe
- Anticipate danger and help your child avoid dangerous situations. Make sure an adult supervises your child at all times, especially when they are in unfamiliar places.
- Always hold your child’s hand to cross the road.
- Know what your child can do physically, and supervise from an appropriate distance.
- Bikes and trikes should not be ridden on the road.
- Helmets and shoes protect heads and feet on bikes and trikes.
- Immunisation (due at 4 years old) helps protect your child from serious infectious diseases.
- Never shake, hit or smack your child – if you feel you might lose control, ask for help.
Ko tō tamaiti i waenganui i te 3 me te 5 tau
He pai ki te mōhio
Te āwhina i tō tamaiti ki te ako me te tipu
- Ka ngahau ki tō tamaiti te wā tākaro me ngā hoa tākaro.
- Me mōhio ia he hirahira ia – kōrerohia atu tōna nui.
- Me aro atu ina pai ia me te whakanui i a ia.
- Whakarongo ki a ia, kōrerohia ōu whakaaro ake mōna – me whai wā kōrua ki te kōrerorero.
- Me kai tahi kōrua.
- Me whai wā motuhake mō ia tamaiti.
- Me pānui ki a ia ia rā – kia whāiti te wā ki te pouaka whakaata/kōpae ataata/tākaro ataata – ka nui te kotahi haora i te rā.
Te tiaki kia ora tō tamaiti
- Me kai ngā tamariki i ngā momo kai rerekē ia rā mai i ngā rōpū kai e whā:
- ngā huawhenua me ngā huarākau
- ngā parāoa me ngā huapata
- ngā mīti iti te mōmona, heihei, kaimoana, hēki, pīni maroke, pī me ngā patapoki
- miraka me ngā hua miraka pēnei i te tīhi me te iokete.
- Me nui ake te kai mā ētahi tamariki i ētahi atu.
- Me whāngai ki ngā paramanawa, kai me ngā inu hauora, pai hoki mō ngā niho, iti hoki te huka hei whakaiti i te tūponotanga o te pirau niho.
- Kāore e tūtohutia te whāngai i ngā inu huarākau, wairanu, waireka hoki (tae atu ki ngā waireka pupū me ngā inu hākinakina).
- Parāhehia ngā niho o tō tamaiti kia rua ngā wā i te rā mā te pani pūkōwhai.
- Hikina te ngutu o runga kia kitea ngā tohu tuatahi o te pirau niho, te pirau taumaha rānei.
- Me heri haere tonu tō tamaiti kia tirotirohia ōna niho, kia whakatikahia rānei mēnā e hiahiatia.
Kia haumaru tō tamaiti
- Tūmanakohia ngā mōreatanga ka āwhina i tō tamaiti ki te ārai i ngā āhuatanga mōrearea: Me mātua whakarite kei te whakahaerehia tō tamaiti e tētahi pakeke i ngā wā katoa, otirā i ngā wāhi tauhou ki a ia.
- Puritia te ringa o tō tamaiti i ngā wā katoa ki te whakawhiti i te huarahi.
- Me mōhio koe ki te kaha ā-tinana o tō tamaiti, ā, ka whakahaere i a ia mai i tāhaki.
- Kaua rawa ngā pahikara me ngā taraihikara e ekehia i runga i te huarahi.
- He ārai wharanga ngā pōtae mārō me ngā hū i runga pahikara, taraihikara hoki.
- Ka āwhina ngā ārainga mate (hei te 4 tau, i mua i te tīmatanga i te kura) ki te tiaki i tō tamaiti mai i ngā mate hōrapa taumaha.
- Kaua rawa e rurerure, e patu, e papaki rānei i tō pēpi – mēnā ki tō whakaaro ka keka koe, me tono āwhina.
Tirohia Kia haumaru, kia ora tō tamaiti
Having fun with a preschooler
Playing, talking and listening
Try to spend time with your child every day without any interruptions. Make playtimes interactive and fun for the child – consider their interests. Giving your child this kind of attention will make them feel special.
Encourage active play and story time. Your local library will have some good ideas about suitable books. Talking and reading together helps language development.
Television, computers, tablets and similar digital devices can be a good resource for children’s learning, but they learn better when an adult shares it with them. Make sure the programmes are suitable for children, and keep total screen time to less than 1 hour a day, and not last thing at night.
Family time during dinner is important for talking and spending time together, so it is better if screens and other electronic devices are off. Limiting such distractions during mealtimes also helps family members be mindful and present during their meal.
There is also a link between learning and movement. The Ministry of Health has published Guidelines for active play for under fives
Behaviour and needs – helping children develop self-discipline
Children do best when they feel loved and valued, are well supervised, and know how they should behave.
Give positive attention. Appreciation, praise and hugs for good behaviour are far more effective than criticising and punishing. If you want to encourage a behaviour, notice it. Let your child know how proud you are of them.
Ignore little things. Choose your battles. Intervene in challenging behaviour only when your child is behaving really badly or is in danger. Giving attention to a child’s bad behaviour usually makes it worse. Children love attention and will sometimes behave in any way that gets it.
Ensure your child understands what is expected of them. Explain to your child exactly what you expect of them and help them to understand the behaviour you want. Be clear and consistent. If your expectations are the same over time, your child is more likely to learn to meet them.
Communicate clearly. When talking to your child, make sure you have their attention. Keep the message short and simple so that they will understand. If you think they can’t hear you, ask your Well Child Tamariki Ora nurse or doctor for their hearing to be checked.
Allow for difference. Every child has their own personality and individual needs. Some are harder to guide than others. Remember that no one is well behaved all the time!
Help children learn from their mistakes. Children – and adults too – make mistakes. Mistakes are opportunities we can all learn from.
Help children learn about feelings. All feelings are OK – it’s how we respond to what happens around us. It’s what we do about our feelings that we need to be able to control.
Children need to know it’s OK to have bad feelings. They also need to learn how to show their feelings without hurting themselves or anyone or anything else. It’s not helpful or healthy to let angry feelings build up. Help children find safe ways to express their feelings. Talk to them about their feelings and their worries. It is never too early to learn that a problem shared is a problem halved.
When you feel angry with your child
Stress, tiredness and frustration can make it hard for parents and caregivers to deal calmly with a crying child, tantrums or challenging behaviour without losing their own control. Almost all parents/caregivers have times when they feel so angry they shout, or want to smack or hit their child. If you feel really angry or upset, give yourself a couple of minutes of ‘time out’ – walk away from them until things cool down. Remember, parents are models for their children. They will want to copy your behaviour to be just like you.
See also Coping with a crying baby
Useful websites
For positive parenting ideas, see:
Never leave a child at home alone
The law says children must be 14 years old before they can be left alone.
The New Zealand Police website has a useful section on this.
When it’s OK for children to say ‘no’
Children need to learn that they can say ‘no’ to an adult or older child in order to keep themselves safe.
They also need to know:
- never to get in a car or go anywhere with someone they don’t know
- the difference between ‘good’ touching and ‘bad’ touching – bad or ‘yucky’ touching is anything that makes them feel uncomfortable
- that it’s always safe for them to tell you things and keep telling you even if another adult tells them not to. They need to know that someone will listen.
Family violence and child abuse
Everyone in a family/whānau should feel safe and nurtured. Any behaviour by a family member that makes someone else feel controlled and fearful is never OK. Abusive behaviours can include following and checking up on you all the time, calling you names or putting you down, slapping or hitting you or your children, controlling your money or where you can go and who you can see.
Violence within relationships has a big impact on the health, development and behaviour of children and all the family/whānau. If you or your children are experiencing violence or abuse, Well Child Tamariki Ora providers can help you get the support you need and link you with support agencies in your community.
If you or your children feel unsafe in any way, you can talk to your Well Child Tamariki Ora nurse or doctor. Someone in your family or whānau may also be able to help and there are community agencies who are there to support you.
Women’s Refuge has a free 24-hour Crisisline at 0800 REFUGE, 0800 733 843 for confidential advice and help in a crisis. The website also has valuable information, including a questionnaire to help you decide if you are being abused.
The Family Violence Information Line 0800 456 450 gives information about where you can go for help if you are experiencing or witnessing violence, or want to change your own behaviour. The phone line is available 24/7 every day of the year.
Are You OK, the website of the Campaign for Action on Family Violence has information, advice and links to various organisations that can help.
If you are concerned for the safety of your children you can ring Oranga Tamariki - Ministry for Vulnerable Children (0508 FAMILY, 0508 326 459) to talk to a social worker. They are trained to help.
If you fear for your children’s or your immediate safety, call 111 for help.
Babies can be tiring and demanding. Never leave a baby alone with anyone who may not be able to cope or may lose control. A single moment of losing control may damage a baby forever. It is especially dangerous to shake a baby, as it can lead to brain damage or death.
KidsHealth has a video called Power to Protect for parents and caregivers about how to cope with the stress of a child’s crying.
If you ever think your baby has been hurt, don’t let fear or pride stand in your way, call 111. It could save your baby’s life
Preschoolers’ teeth
Your child will probably want to brush their own teeth by now. You should continue to help your child brush their teeth until they are 8 or 9 years old. Brush twice a day with half a pea-sized amount of regular-strength fluoride toothpaste and encourage your child to spit out the toothpaste after brushing and not rinse with water. Make sure that your child is not using too much fluoride toothpaste, or eating it.
Enrol your child with the Community Oral Health Service or a dentist and ensure that you or other family members or whānau accompany your child to appointments. Regular dental visits are vital, not only to prevent potential dental problems but also to reduce the stress and pain of dental decay.
If your child accidentally bumps their teeth, it is important that you take them to a dental or oral health professional in the Community Oral Health Service or a dentist, even when the teeth still look all right. The oral health professional can check that no damage has been done to the nerves or to the developing teeth. You may need to be referred to a private dentist who carries out ACC funded treatment if treatment is required. A co-payment may then be required.
Contact your Community Oral Health Service for free advice and treatment – call 0800 TALK TEETH, 0800 825 583
Toilet training
About 1 in 10 of all 5 year olds still can’t help wetting the bed at night. Some may have the occasional wetting during the day too. Boys often take longer to be dry at night than girls. Getting upset and angry won’t help. Just show them you are really pleased when they are dry all night.
Sometimes a simple star chart can help them be dry at night, but don’t make it too hard for them to get a reward to start with. Use rewards like special time or an outing rather than sweets or other treats.
Sometimes children who are dry at night start wetting again. This can be due to stress (such as the arrival of a new baby or moving house), but it should settle down quickly with positive encouragement and support. If it persists or you have concerns about it, ask your Well Child Tamariki Ora nurse or doctor for advice or call PlunketLine 0800 933 922 to talk to a Well Child nurse.
Looking after yourself
When you’re a new mother you need time to develop a relationship with your baby. As they grow you’re more likely to enjoy being a parent if your needs are met too.
Eating well
What you eat will have a big effect on how you feel during the day and how well you sleep. When you are eating well, you are looking after yourself and your baby too. Try not to miss meals and drink plenty of water. Coffee may give you a short boost, but it doesn’t replace a meal. Frequent healthy snacking during the day may work better for you.
HealthEd has useful booklets on healthy eating for women and families:
- Eating for healthy breastfeeding women (HE1806)
- Eat healthy food and move more every day (HE1333)
-
Healthy eating, active living (HE1518)
- Eating for healthy vegetarians (HE1519)
For information about keeping yourself healthy while breastfeeding, see Mothers need to look after themselves too and Breastfeeding is best for your baby
Sleep
Getting the sleep you need is not easy with a new baby or a very young child, but they need you to be healthy and rested. Sleep is one of the most important parts of looking after yourself and your baby. It’s important for milk production too.
Asking for help with chores and childminding while you sleep is not being lazy.
Signs of sleep deprivation include being grumpy, and being more emotional, stressed, and hungry (or less hungry) than usual. People can become clumsy and find it hard to focus, remember things or communicate. Sometimes sleep deprivation can look a lot like postnatal depression (see Postnatal depression). If your feelings persist, talk to your Well Child Tamariki Ora nurse or doctor.
Things you can do to get more sleep
Sleep when your baby is sleeping. If you can’t do this, use some of the time to do something relaxing or one thing you actually want to do – like have a long bath or shower or catch up with your online friends.
Ask for help. If you have a partner, they may be able to bring your baby to you for a night feed and put the baby back in their own bed afterwards.
The light from screens wakes up your brain and makes it harder to go to sleep. It’s best to avoid them for an hour or so before you go to bed.
Tea, coffee, cola, energy drinks and chocolate all contain caffeine, which may keep you awake. If you’re really sensitive to caffeine, it’s best not to have these later than early afternoon. Some pain medication contains caffeine – check the label. If you are breastfeeding and taking in a lot of caffeine, your baby will get it through your milk, and it might make them hard to settle.
Cigarettes, alcohol and other drugs can also affect how well you sleep.
It is best for both you and your baby if you can stop or reduce smoking while you are breastfeeding as your baby will get nicotine and other harmful substances through your milk.
Quitline provides help, advice and resources for stopping smoking.
Other tips may work well:
- Keep well hydrated – drink plenty of water during the day.
- Gentle exercise, such as an evening walk, may lift your mood and help you sleep better.
- Make a list of important tasks. Knowing that you can always check what you need to do will help you relax and feel on top of things.
- Try having an earlier bedtime. Many babies sleep best during the first few hours of the night, so getting your rest at the same time can help you get a few extra hours of sleep as well.
- Maybe older children could stay with relatives or friends some nights. As well as giving you a break, this would give them the chance to spend some special time together.
Ask for help – and accept it
It’s OK to accept help from others, and to ask for help yourself. Often it’s the help with the small, everyday things (childcare, meals, errands, or housework) that makes a big difference.
Stress, worry, anxiety or postnatal depression
You can expect a range of feelings when you’re a new parent, including anxiety about how you are coping, and worry that you are not ‘good enough’. You might also feel sad or angry if your baby’s birth has not gone according to plan or if you don’t feel well supported. These feelings are normal.
Many mothers experience the ‘baby blues’ for a few days after birth. The ‘blues’ make you feel teary, anxious and down but usually go away by about the tenth day after the baby arrives.
Up to half of all birthing parents will experience some level of emotional or mental distress that is ongoing after birth including depression or anxiety. This is more likely if you or a close family member have experienced these or similar difficulties in the past, or during pregnancy. Other contributing factors can be stress, loneliness, isolation, lack of support (practical and emotional), a difficult or premature birth, the birth of a pēpi with serious health problems, challenges with breastfeeding, or relationship issues or violence.
You may feel worthless, hopeless and/or sad and have changes in your eating and sleeping patterns. You may blame yourself when things go wrong, feel anxious, panicky or overwhelmed, and in more severe cases have thoughts of suicide or hurting your pēpi. You might not feel close to your pēpi or to other whānau members. Sometimes these feelings can emerge suddenly and unexpectedly. At other times, your moods may swing for no obvious reason. If these feelings don’t go away in a few days or if you or your whānau are worried about how you feel, talk straight away to your Lead Maternity Carer, Well Child Tamariki Ora nurse, doctor or someone you trust.
Mental distress, including anxiety and depression, is treatable and getting support early leads to the best outcomes. Your preferred provider will be able talk to you about treatment such as counselling or in some cases medication. They will also know what help is available in the community.
If you’re worried about postnatal depression or mental or emotional distress of you or your partner talk to your doctor, midwife, Well Child Tamariki Ora nurse or someone you trust. Alternatively, you can call:
- Healthline 0800 611 116
- PlunketLine 0800 933 922 or visit a local Plunket Family Centre (to find one, see Plunket near me » Whānau Āwhina Plunket)
- If you want to talk (kōrero) to a trained counsellor about how you’re feeling, or you’ve got any questions, you can call the Depression Helpline 0800 111 757 or Need to talk? Free call 1737 or free text 1737 any time for support from a trained counsellor.
For more information on mental distress during pregnancy or after your pēpi is born, you can visit:
- PADA - Perinatal Anxiety & Depression Aotearoa
- Navigating parenthood | Depression and Anxiety | Welcome to a Brand New Day
Read or order a general resource on mental health from There is a way through: A guide for people experiencing stress, depression and anxiety | HealthEd
Relationships
It can be easy for new mothers to feel they have to do everything on their own, especially if they are single parents or don’t have friends or family/whānau nearby. There will be other parents/caregivers of young children you can share things with – if you went to an antenatal group or have joined a Plunket or playgroup, you will know some already – and neighbours are often happy to help in some way. Plunket near me will help you find a group in your area. Your local library, community centre and community noticeboards are also good sources of information. Birthright offers valuable help, advice and support to single-parent families.
Having a baby is a big lifestyle change. Your house won’t be the same, and that’s normal. Here are some ideas to try:
- Decide what tasks are really important and ask family/whānau, friends and neighbours for help. It’s OK to leave a pile of washing on the couch for a few days!
- Take some time for yourself – do something of your own. Give yourself some little treats. Time out with friends, a bath, or something as simple as reading a magazine, going for a walk or watching some TV can make it easier to cope.
- Spend some time just with your partner, as well as shared family time. It is good for partners, family/whānau and friends to be involved in some child and health care too. If you have other children, they will want to be involved with your baby as well.
- See if you can manage some individual time with each child.
- Talk, together with your family/whānau, about bedtimes, food and other household matters.
- Talk to your Well Child Tamariki Ora nurse or doctor about your family/whānau’s health needs.
Partners are needed too
All partners who share in raising a child need to be able to bond with them in their own right, especially in the early stages.
If they are working outside the home, parental leave is very important. It allows them to give much-needed support and get closely involved in caring for their children.
For more information on parental leave, go to Parental leave | Employment New Zealand
With a new baby in the home, partners have a vital role in keeping normal family life going – dealing with day-to-day arrangements, attending to the care of other children, supporting the mother, and arranging other help as needed. This frees the mother from household cares so that she can concentrate on establishing breastfeeding and getting to know the baby and the baby’s needs.
Partners sometimes feel they don’t know how to do this. They may not be sure what is most helpful and how to provide it. They can also feel excluded or criticised when professionals ignore them and dismiss their ideas and needs.
Work and financial pressures can be another source of stress. Partners may feel responsible for resolving money problems, even when these are outside their direct control. They may not know how to offer support to the mother during the ‘baby blues’ or when she feels she is not coping with her baby. They may feel that it is hard to get it right.
Partners too often struggle with lack of sleep and the lifestyle changes a new baby brings, and may also experience depression. A new baby changes a couple’s relationship in ways that partners may feel as a loss. They may need help, but are less likely to ask for it, and may be uncomfortable sharing ‘family business’ with others.
Useful websites
Organisations such as Kidz Need Dadz | Support & Education to Strengthen Father-Child Relationships provide advice and support specifically to partners. Parenting Support For Dads | Great Fathers Mana Mātua is another valuable source of information and advice.
Or view resources for dads and postnatal depression at Depression in Fathers - PADA - Perinatal Anxiety & Depression Aotearoa
Find some ways to support your partner at Supporting your pregnant whānau member
Keeping your child healthy and safe
- Protecting your baby from SUDI – make every sleep a safe sleep
- Help your child to be healthy and strong – be smokefree, breastfeed and immunise
- Choking, strangling, suffocating
- Poisons
- Burns, fires, scalds
- Cuts
- Falls
- Road and car safety
- Medicine use
- Water safety
- Sensible sun exposure
- Allergies
- Infant mental health and brain development
- Family violence and child abuse
- Shaken baby
- Infectious illnesses
- Ear problems
- If you’re concerned about your child’s speech or language
- Skin infections and skin care
- Eczema
- Looking after your child’s teeth
- Safe drinking water
- You can support a safe community for your child
Protecting your baby from SUDI – make every sleep a safe sleep
Sudden Unexpected Death in Infancy (SUDI) is a risk to babies until they are about 12 months old, but most SUDI is preventable. There are things we can do to protect our babies.
Although for some babies the cause of death is never found, most SUDI happens when a baby is sleeping in an unsafe way.
The safest place for all babies to sleep at night is in their own cot, bassinet, pēpi-pod® or wahakura, close to parents/caregivers and in the same room.
Babies may begin to roll over from their back to their front when they get to 5 or 6 months old. You don’t need to try and stop this from happening, as long as their cot is free of things that might suffocate them such as pillows, large soft toys or cot bumpers.
You can help protect your baby from dying suddenly in their sleep by:
- making sure your baby is in their own bed for every sleep (and in the same room as parents/caregivers at night)
- making sure your baby is on their back for every sleep
- keeping your baby’s environment smokefree and vape free from the start
- breastfeeding your baby
- immunising your baby on time
See Safe Sleep For Your Baby | KidsHealth NZ for more information.
Make every sleep a safe sleep
Always follow these safe sleep routines for your baby and your baby’s bed.
Make sure your baby is safe
Sleep your baby on their back to keep their airways clear for breathing. Put your baby to sleep in their own bed, not with an adult or another child who might accidentally smother them.
Always make sure your baby has a parent/caregiver who is alert to their needs and free from alcohol or drugs. Just as you would nominate a sober driver, every baby and child needs a sober caregiver.
Make sure your baby sleeps in their own bed
For the first 6 months, the safest place to sleep at night for all babies is in their own cot or bassinet, close to parents/caregivers and in the same room.
If you choose to sleep in bed with your baby, put them beside you in their own baby bed – for example, a pēpi-pod® or wahakura. This may help reduce the risk of your baby suffocating while they are asleep.
Information about using a pēpi-pod® or wahakura is available online at Pēpi-pod or ask your Lead Maternity Carer or child health nurse or see SUDI Prevention | SUDI Prevention Coordination Service
If you are out somewhere, make sure your baby has a safe place to sleep. Take your wahakura, pēpi-pod®, portacot or bassinet with you, and use it on a flat surface. Tilting the sleep device may cause your baby to roll and suffocate.
It is never safe to put your baby to sleep in an adult bed, on a couch or on a chair.
Car seats or capsules protect your baby when travelling in the car. Although your baby may fall asleep in the car seat, it’s best not to use it as a cot or bassinet.
If you don’t have a baby bed, ask your Lead Maternity Carer or Well Child Tamariki Ora nurse. If you are on a low income, you may be able to receive a Special Needs Grant from Work and Income to buy a bed.
For more information visit Work and Income or call 0800 559 009
Make sure your baby’s bed is safe
Your baby’s bed needs a firm flat mattress that fits snugly so your baby can’t get into any gaps between the frame and the mattress.
Babies may begin to roll over from their back to their front when they get to 5 or 6 months old. You don’t need to try and stop this from happening, as long as their cot is free of things that might suffocate them such as pillows, large soft toys or cot bumpers. There should be nothing in the bed that could cover their face or lift their head.
Make sure that cots are assembled correctly. The tops on the corner posts of wooden cots may need to be sawn off so your child can’t hang themselves by their clothing. Consumer Affairs New Zealand states that spaces between the bars of the cot must be between 50 mm and 95 mm. Try to make the spaces closer to 50 mm if you can.
If you have a cot with adjustable levels, make sure you lower it before your infant can pull themselves up (about 9–10 months).
The cords for blinds and curtains are a danger. Put the cot away from the window so your child can’t reach them. For more on preventing choking and strangling, see Choking, strangling, suffocating
Make sure your baby is healthy and strong
Being smokefree during pregnancy and after is best for your baby. If a mother smokes during pregnancy, poisonous chemicals affect the growing baby. This weakens them after they are born so that they are unable to react as strongly to situations such as accidentally having their face covered. After your baby is born, it is important to keep your home and car smokefree and vape free and make sure that others don’t smoke around the baby. This will help your baby grow strong and healthy.
Feed your baby only breast milk for the first 6 months and keep breastfeeding for the first year. Make sure your baby is immunised on time.
If you find your baby not breathing, call for help, and begin rescue breathing (CPR) immediately.
Help your child to be healthy and strong – be smokefree, breastfeed and immunise
Being smokefree and vape free through your pregnancy and having a smokefree and vape free home and car will help keep your child healthy and strong. Make sure friends and family/whānau don’t smoke or vape around your child, either.
Breast milk is the only food your baby needs for the first 6 months. Some new mothers need help as they and their baby learn to breast feed in the early days and weeks. Keep breastfeeding after your baby starts solids, during the first year and beyond.
Immunisation protects your baby and toddler from several serious diseases. Make sure your child is immunised on time. See Immunisation.
Choking, strangling, suffocating
As your baby becomes more mobile around the floor and starts to eat solid food, there are some things you need to think about to keep them safe.
Is there anything small on floors and furniture?
Small pieces of hard food, like some raw fruits and vegetables, nuts or small, hard sweets, can cause choking.
Your child will be safest if they sit while eating and an adult stays with them.
Do household objects and toys have any small, sharp or loose pieces? Check them often.
There are choking and strangling risks in the bedroom too. Make sure that cots are assembled correctly. The tops on the corner posts of wooden cots may need to be sawn off so your child can’t hang themselves by their clothing.
The cords for blinds and curtains are a danger. Put the cot away from the window so your child can’t reach them.
Check that bars on cots, playpens, stairs, verandahs, and stair guards are secure and vertical. Consumer Affairs New Zealand states that gaps between the bars of the cot must be between 50 mm and 95 mm. Try to get one with the gaps closer to 50 mm if you can. This will prevent your child getting through or getting any part of themselves caught in the bars.

[Image showing gaps between stair railings]
Cot mattresses should be clean and dry and fit snugly in the cot, with no gaps around the edges.
Think about the risks of choking when choosing clothing for your child. Clothing should be close-fitting, with no long ribbons or open weaves, and no loose ties near the neck.
Take your child’s bib off for sleeping.
Tie plastic bags in knots and keep them out of reach.
Useful websites
Keeping kids safe has safety information about products that can cause harm to babies and young children.
Poisons
Lead
Check for lead paint on older furniture and toys. It can poison babies and young children. Talk to your Well Child Tamariki Ora nurse, your doctor, or a health protection officer (HPO) at your local Public Health Unit before removing paint. The HPO will test it for lead and advise you about removing it if necessary.
You can find information on lead-based paint and lead poisoning at Lead poisoning The page gives information on sources of lead and the symptoms of lead poisoning.
Other poisons
Look for child-resistant closures on household cleaners, poisons and medicines. Ask your pharmacist for child-resistant closures on all medicines and do them up tightly – remember that they are child-resistant, not child-proof!
Keep all household products and medicines in their original labelled containers – never put poisonous products in drink or food containers.
Lock all household products and medicines out of sight and reach. Always read the label before using the product, even if you have used it before. While you are using anything poisonous, always keep it well out of your toddler’s reach.
Make sure your child knows not to eat any plants, berries, mushrooms, etc that they find. Check for poisonous plants in your garden and house and get rid of them.
You can download Plants in New Zealand poisonous to children from the Landcare Research website. The poisonous plants page also has other links to information on poisonous plants.
Keep the phone number for the National Poisons Centre close to the phone – 0800 POISON, 0800 764 766
Burns, fires, scalds
Check the temperature of your child’s food and drink. Take care with microwave heating, as food can heat unevenly and get too hot very quickly. Microwaves are not recommended for warming formula because they can easily overheat or heat unevenly and burn the infant's mouth and throat.
Make sure that electric jugs and kettles have a wide base and short or curly cords.
Keep all hot things out of reach.
Don’t hold your child while you have a hot drink.
Have a stove guard fitted and use the back cooking elements. Turn pot handles away from the front.
Have guards fitted to walls around fires and heaters.
Children will copy you so keep lighters, matches and candles out of reach.
Have a smokefree and vape free home and car, and don’t keep lighters and matches in the car.
Make sure heaters can’t tip over. Don’t have clothing near or on heaters.
Never leave bar heaters, or heaters without thermostats, on in the room where your child sleeps.
Put safety plugs in electric sockets when the sockets are not being used.
Use nightwear that is labelled as low fire risk. Cotton material burns very easily.
Keep your hot tap water at around 50°C – see if it’s OK to hold your hand under the running tap for 5 seconds.
When you are bathing a baby, put cold water in the bath first, then add the hot water. Test the heat of the water before you put your baby in it – use the inside of your wrist.
Have a fire extinguisher and/or fire blanket correctly located in your kitchen and make sure you know how to use them. The Fire and Emergency NZ website has detailed advice on fire safety in the home. The page also has a link to a home fire safety checklist. The website also has advice on making an escape plan.
Smoke alarms in your home will help to wake you if there is a fire. They are recommended in all bedrooms. Make sure you check their batteries twice a year. Your local fire service can advise you on the best types to get.
Cuts
Sharp corners on low tables may need rounding off, or covering until your child is bigger.
Have safety film, wooden bars, or safety glass on glass doors and on windows near floor level, especially upstairs windows. Bright stickers at a child’s eye level on large areas of glass can help.
Keep knives and scissors out of reach.
Falls
Be proactive about your child’s safety. Know what they can do physically. Check the environment for hazards and supervise from an appropriate distance. At family gatherings and other occasions when small children are present and alcohol is being drunk, make sure that at least one adult who isn’t drinking keeps an eye on the children.
Make sure your baby can’t fall off things.
Put bars on cots, playpens, stairs, and verandahs. Stairguards need to be upright and well secured. If they have bars, the gaps between the bars should be smaller than 95 mm. Consumer Affairs New Zealand states that gaps between the bars of cots must be between 50 mm and 95 mm. Try to make the gaps closer to 50 mm if you can.
Keep stair and door guards in place.
Place furniture away from windows.
Make sure heavy furniture (such as bookcases) and other large objects are secured so that they cannot fall. This is good for earthquake safety and prevents children pulling a heavy object on top of themselves.
Have safety catches on windows.
Make sure your child plays well away from glass doors and windows.
Outdoor play equipment should have a soft surface, such as bark chips, underneath it.
Play equipment needs to be lower than adult height.
Crawling backwards is a safe way for your baby to get downstairs, if someone is with them.
Baby walkers are not safe. It is better not to use them.
Road and car safety
Children are especially vulnerable to injury in car crashes. The seats and safety belts installed in most vehicles are designed to protect an average-sized adult. Because children are smaller and have different body shapes, they need more protection to keep them safe in a car. It is important to use a car seat for every ride. Car seats can be hired. Ask your Well Child Tamariki Ora provider or nurse about local hire services.
Under New Zealand law, all children travelling in cars must be in a child restraint until their seventh birthday. However, height is very important in the use of a child restraint – to be as safe as possible, children should use a child restraint until they are 148 cm tall. If your child is 148 cm or taller, they must still wait until they are 7 years old before they can use an adult seatbelt.
If your child is 7 years old but is not yet 148 cm tall, it is safer to keep them in the restraint until they are that height. The car seat must be an approved child restraint appropriate for your child’s age and size, and it needs to be fitted correctly.
It is the driver’s responsibility to make sure any child travelling in their car is correctly secured in a child restraint. Always follow the manufacturer’s instructions when installing a car seat.
The back seat is the safest place for any child. Rear-facing restraints should never be used in the front seat where there is an airbag.
When you are buying or hiring a child restraint, always try it in your vehicle to make sure it fits well. Check too that the seat you are looking to buy or hire is right for your child. Child restraint technicians at Plunket, your rental scheme or your retailer will be able to help you make the right choice.
Stages of child restraint
There are three stages of child car restraint.
Stage 1: Infant restraint (rear-facing)
Babies are better protected in a rear-facing restraint. This can be a baby capsule or a convertible car seat used rear facing.
Keep your baby facing the back of the car until they are 2 years old. Babies have outgrown the restraint when their head reaches within 2 cm of the top or they are over the recommended height and weight for the restraint. If the restraint is convertible, it can then be adjusted to a front-facing restraint. Always follow the manufacturer’s instructions.

[Rear-facing child restraint]
Stage 2: Front-facing child restraint
Your child should stay in a correctly fitted child restraint until they have outgrown it. This will be when their eye level has reached the top of the restraint and they are over the maximum recommended weight. Check the manufacturer’s instructions.

[Front-facing child restraint]
Stage 3: Booster seat
A booster seat is designed to improve the fit of the safety belt and raise the child to window level. To be used safely:
- the diagonal belt must go over the shoulder and not sit across the child’s neck
- the lap belt must sit low, touching the top of their thighs.
You may be able to hire an approved child restraint from Plunket, some Well Child Tamariki Ora providers, some baby shops, community groups and some rental-car companies.

[Booster seat]
For more information on how to correctly install child restraints and on legal requirements see the NZ Transport Agency Waka Kotahi Child restraints save lives | NZ Transport Agency Waka Kotahi Requirements for using child restraints in New Zealand | Waka Kotahi NZ Transport Agency (nzta.govt.nz) You can also go to Child Car Seats | KidsHealth NZ for advice on purchasing and fitting car seats.
Other safety tips to think about
Always check that the driveway is clear before getting into your car and driving out. Check and check again, especially if you are reversing – you may not be able to see a small child who is close to your car. It’s safest to ask another adult to watch the children as you are driving out.
Make sure you know where your children are when visitors are using your driveway.
Fence outdoor play areas and make sure unsupervised children can’t get into the garage or work areas, or onto your driveway or the road.
It is never too early to start teaching children about road safety. Children learn by watching you. Show them how to be safe on and near the road, and to watch for cars coming in or out of driveways.
Holding hands with an adult to cross the road is a ‘must’ rule. A child under the age of 8 is not mature enough to cross the road alone.
Getting children in and out of a car on the footpath side is safest, so consider fitting the child restraint on the left side of the car.
If you are picking your child up from school, it is best to park and then walk to meet them at the school gate. Children sometimes rush across the road to someone they know without looking for traffic. If your child is under 10, they should have an adult with them when travelling on a school bus.
Children under 10 should also have an adult with them if they are riding a bicycle on the road. Make sure they wear a cycle helmet. Using a helmet from the beginning will help them choose to continue using one as they get older.
Medicine use
Always check with your doctor or pharmacist before you give any medicine to your child. It will only work if it is the right medicine for your child’s illness and is used correctly. Make sure you give the right dose. Pharmacies have special droppers for giving liquid medicines to children. It is also important to ask the pharmacist for child resistant caps for medicines for your family.
Medicine that is not used correctly will not work and may even cause harm. Medicine that is right for one child may be wrong for another. It is not safe to give medicine on advice from friends or family/whānau.
Always make sure your child finishes the whole course when they are prescribed an antibiotic.
Talk to your doctor or pharmacist on the telephone if you can’t visit.
Water safety
Babies and toddlers must be within sight and reach of an adult at all times around water. Small children can drown in very small amounts of water, including buckets and baths.
Check that:
- Anything that holds water is safely away. Keep lids on nappy buckets and make sure they are out of reach.
- The toilet door is always closed. Think about putting an automatic door closer on bathroom doors.
- Swimming pools and spa pools are fenced and safely gated. Most toddler drownings happen in the family’s own pool or in a pool owned by friends. The law requires home swimming pools to be fenced and safely gated. Spa pools must have a lockable lid.
- A responsible adult is watching children around water at all times.
For more information see Safety guidance for pool owners or Water Safety New Zealand.
If you need to go away from your child’s bath or paddling pool, take your child with you. Drain paddling pools when they are not in use.
At public pools, actively supervise your child. This means staying in arm’s reach of preschoolers.
Do not rely on bath seats and other flotation aids to keep your baby or toddler safe, as they can tip over and trap the child under water.
Teach children to stay away from the edge of pools and rivers and to wait for you or another adult before getting in the water.
Always make sure everyone is wearing a correctly fitting lifejacket when out on a boat or other watercraft.
Sensible sun exposure
Sun protection is particularly important for babies and toddlers. Babies should not be exposed to direct sunlight, particularly between 10 am and 4 pm from September to April.
September to April (including the daylight saving months)
Keep toddlers out of the sun as much as possible between 10 am and 4 pm.
Toddlers are likely to make enough vitamin D from sunlight if they are outdoors for short periods before 10 am and after 4 pm.
May to August (the cooler months)
In winter, it is generally safe and advisable for toddlers to spend some time in the sun.
Shade, protective clothing, broad-brimmed hats, and sunglasses are the first line of protection against sun exposure in infants and young children. When they need more sun protection, use broad-spectrum sunscreen with at least SPF30+. Wipe it on thickly – don’t rub it in hard. Avoid the eyes and hands – remember that babies rub their eyes, so sunscreen on their hands could hurt their eyes.
For infants and children with sensitive skin, use zinc- or titanium-based (non-absorbable) sunscreens. If you use other sunscreens, do a patch test to check for sensitivity – put a little on your child’s skin, leave for a few hours and check if the skin shows any kind of reaction.
However, it is best to keep babies out of direct sunlight.
Vitamin D
Children need vitamin D for strong bones. Breast milk is the best food for young babies but it is not a good source of vitamin D. Our bodies make vitamin D when our skin is exposed to sunlight, but babies can’t safely get the vitamin D they need from the sun because their skin burns so easily.
Babies who are at high risk of vitamin D deficiency can be prescribed vitamin D. If you think your baby is at high risk, talk to your Lead Maternity Carer, Well Child Tamariki Ora nurse, or doctor.
Vitamin D and your baby has useful information on vitamin D, the risk factors for deficiency, and giving supplements. You can also go to Health Information and Services and enter Vitamin D in the Search box.
Safety warning
Baby oil (or any other oil, such as coconut oil) is not a sunscreen and will not protect your child from sunburn!
Allergies
Allergies are common in childhood and may begin with the development of food allergies in children under 12 months old. Milk (dairy), eggs and peanuts are the most common food allergies in this age group, but fish, shellfish, tree-nuts, sesame, wheat and soy can also be a problem. Many children grow out of their food allergies in late childhood, although allergies to peanuts, tree-nuts, fish and shellfish tend to continue into adulthood.
Eczema is a common health problem in infants. It occurs in around 1 in 5 babies and young children. Most children with eczema do not have food allergies, but food allergy is more common in babies with eczema and a family history of food allergy. For more on eczema, see Eczema
The children of parents with allergies are more likely to develop allergies themselves, but no one knows why some babies develop allergies while others don’t. Avoiding the foods most likely to cause allergies while you are pregnant and breastfeeding won’t prevent your baby from developing allergies, but the best thing you can do is breastfeed for at least the first 6 months and not be exposed to cigarette smoke.
It helps to continue to breastfeed while you are introducing solid foods, especially the foods that most commonly cause allergies. However, if you delay introducing these foods, it may increase the risk that your child will develop allergies to them. There is no reason to delay the introduction of foods that most commonly cause allergies (see the list of foods above). See More information on feeding your baby
Some children may show signs of an allergy within minutes of eating the problem food. Symptoms of allergy may include:
- swelling of lips, face, eyes
- hives or welts on the skin
- itchy, red eyes; sneezing and/or a runny nose
- abdominal pain, vomiting and diarrhoea.
Some children have severe reactions to food, called anaphylaxis, which can affect their breathing and/or circulation. The child may cough and wheeze, or their tongue and airway may swell, or they may become very pale and collapse. This is a medical emergency – call 111 immediately for an ambulance.
If you suspect your child has food or other allergies, talk to your Well Child Tamariki Ora nurse or see your doctor for further advice.
More information about allergies can be found on KidsHealth and Allergy New Zealand
Infant mental health and brain development
Children need to be in a safe and nurturing environment to become happy and healthy adults. For their mental health they need love and warmth, talking and listening, guidance and understanding, limits and boundaries, consistency in behaviour from the adults around them, knowledge that actions have consequences, and a safe and secure world.
Children’s brain development is an important factor in their infant years. A baby’s brain is fully grown at birth, but the brain cells are poorly connected to each other. Over the next 3 years the brain grows more complex and capable. Consistent nurturing and positive rich experiences during this time are likely to result in flexible, responsible, empathetic and intelligent adults. Adults who have experienced neglect, chaotic environments, violence and abuse often find it difficult to form caring relationships and manage their emotions and impulses.
For more information about infant mental health and brain development, go to Raising Children
Family violence and child abuse
Everyone in a family/whānau should feel safe and nurtured. Any behaviour by a family member that makes someone else feel controlled and fearful is never OK.
Family violence has a serious impact on children’s healthy development and behaviour, which can last their whole life.
Are You OK | Family Violence Information and Support has plenty of information, advice and resources, and gives links to various organisations that can help.
If you or your children feel unsafe in any way, you can talk to your Lead Maternity Carer, Well Child Tamariki Ora nurse or doctor. Someone in your family or whānau may also be able to help and there are community agencies who are there to support you.
You can also contact Oranga Tamariki Ministry for Children (0508 FAMILY, 0508 326 459) and talk to a social worker.
If you fear for your immediate safety, call 111 for help. For more information, see Keeping your child healthy and safe
Stress, tiredness and frustration
Stress, tiredness and frustration can make it hard for parents and caregivers to deal calmly with a crying child, tantrums or challenging behaviour without losing their own control. See Coping with a crying baby
Other sources of help
Women’s Refuge has a free 24-hour Crisisline at 0800 REFUGE, 0800 733 843 for confidential advice and help in a crisis. The website also has valuable information, including a questionnaire to help you decide if you are being abused.
The Family Violence Information Line 0800 456 450 gives information about where you can go for help if you are experiencing or witnessing violence, or want to change your own behaviour. The phone line is available24/7 every day of the year.
Are You OK | Family Violence Information and Support has information, advice and links to various organisations that can help.
You can also find helpful information on the KidsHealth website.
Shaken baby
Never, ever shake a baby, as you could easily hurt them. Shaking a baby can cause brain injury or death.
If your baby won’t stop crying, it is OK to put them down gently in a safe place, close the door and take a break. Do not pick up the baby again until you have calmed down and are ready to comfort them.
There is a national programme to teach new parents about the dangers of shaking a baby, with help and advice on what they can do when the baby cries. For more information, see KidsHealth.
Watch the Power to Protect video for parents and caregivers about how to cope with the stress of a child’s crying, and the consequences of shaking a baby, at Never Ever Shake A Baby | KidsHealth New Zealand's Trusted Voice On Children's Health
For suggestions on coping with stress, tiredness and frustration, see Coping with a crying baby and Looking after yourself
Infectious illnesses
If you suspect any of these illnesses in your family/whānau, tell your doctor.
Immunisation prevents these illnesses.
| Early signs | Time from first contact to first sign of illness | Infectious to others | What to do |
|---|---|---|---|
Hepatitis B
|
6 weeks to 6 months | Months
A few are infectious |
See your doctor for testing. |
Measles
|
7–18 days
About 10 days |
From 5 days before rash appears to 5 days after rash appears | Other children who have not had measles and are not fully immunised should be kept home for 2 weeks. |
Mumps
|
About 16–18 days
About 18 days |
For 1 week before signs to 9 days after first signs | Other children can go to school. |
|
Pertussis (whooping cough)
|
About 7 days
About 10 days |
For 3 weeks from first signs if not treated with antibiotics. If the child has antibiotics, until 5 days of the treatment |
If other children in the house are not fully immunised, keep at home for 2 weeks. Keep babies and toddlers right away from patient (OR keep home until 5 days of course of antibiotics |
Rotavirus
|
24–72 hours | From first day of illness until about 8 days later | Make sure your child has plenty to drink. Wash and dry your hands well after changing nappies and going to the toilet, and before touching food. Keep child away from others – they shouldn’t go to childcare while they are infected. |
Rubella
|
About 16–18 days | From 7 days before rash until 7 days after rash started |
Pregnant women should avoid contact with rubella, but if contact occurs, see your doctor. |
Chickenpox (varicella)
|
About 14 days About 15 days |
From up to 5 days before first lot of blisters until blisters have crusted (usually about 5 days after last blisters appear) |
Other children can go to school. |
For more information about these illnesses, see Infectious Diseases (HE1215)
Other non-funded vaccines:
Talk to your doctor or nurse about other non-funded vaccines that are available and recommended for healthy babies and young children, including influenza. There will be a charge for these vaccines.
Other funded vaccines:
Some babies and young children with chronic conditions may be offered other or additional funded vaccines.
Some extra vaccines that aren’t currently on the schedule may be recommended if your child is considered ‘high-risk’ or you’re travelling overseas.
Ear problems
Ear problems can stop children from hearing and learning.
Your child should have the regular ear and hearing assessments offered by your Well Child Tamariki Ora nurse or doctor with the health assessments in this book. These assessments can pick up a health problem like glue ear, which doesn’t always cause earache and so may not be noticed without the assessment.
Earache
Earache is usually caused by an infection and often accompanies a cold or sore throat.
Earache is painful and should be treated quickly. Your child may have an ear infection if they keep crying or are grizzly, they keep touching their ear over and over again, or they get a runny ear. They may also have a cold.
If you can’t settle your child, phone your Well Child Tamariki Ora provider, nurse or doctor or Healthline 0800 611 116 right away. Lifting your child’s head up above the level of their chest will help relieve the pain.
If your child is on medicine for an ear infection, make sure they keep taking the medicine until it is all gone, even if they no longer show signs of a sore ear.
Glue ear
Glue ear happens when the middle ear is filled with mucus or fluid. It usually gets better without causing problems, but may recur with every cold. If you think your child has hearing or behaviour, talk to your Well Child Tamariki Ora nurse or doctor about a hearing (audiology) test. After your child has been treated by a doctor or specialist, their hearing will usually be OK again.
Possible signs of glue ear
Baby
- They don’t seem to be interested in sounds.
- They are crying, cross or not sleeping.
- They have a cold or fever.
Toddler or preschooler
- They don’t hear you.
- They are late learning to talk.
- They are cross, and upset with everyone.
- They have had earache several times before.
- They snore, and breathe through their mouth.
- They have a greenish, runny nose.
You can help prevent glue ear by:
- breastfeeding your baby
- making sure your baby is in an upright position while bottle feeding
- having a smokefree and vape free home that is warm and dry (and a smokefree and vape free car).
If you think your child might have glue ear, see your Well Child Tamariki Ora provider, nurse or doctor straight away.
See also Ear infections, earache and glue ear - HE1414 – HealthEd
If you’re concerned about your child’s speech or language
Children develop language skills at different rates, but if your child has speech difficulties, the sooner these are found and treated, the better your child’s learning and achievements will be.
For more information, see Speech & Language | KidsHealth NZ
In the table below, the * symbol describes a communication skill that most children achieve by the age shown in the first column. If your child has not achieved one of these skills by the age shown, ask your Well Child Tamariki Ora nurse or doctor for a review. Problems with speech and language development can also be a sign of hearing difficulties – for example, your child may have glue ear and may need their hearing checked.
Age: 6 weeks old
Understanding:
- Listens to speech and noises around them. Startles at loud noises.*
Speaking/communication:
- Makes eye contact and smiles in response to others.*
Age: 3 months old
Understanding:
- Turns to the sound of a familiar voice.
- Likes listening to stories.
Speaking/communication:
- Makes cooing, gooing noises.
- Uses different cries for different situations.
- Laughs. *
Age: 6 months old
Understanding:
- Responds to changes in tone of voice.
- Enjoys rhythm and music.
Speaking/communication:
- Makes “p”, “b” and “m” sounds.
- Speech-like babble.
Age: 12 months old
Understanding:
- Listens when spoken to.
- Turns and looks at your face when called by name.
- Understands common words like "Daddy", "Mummy" and "car".
- Follows simple, single-step instructions.
Speaking/communication:
- Uses speech-like noises to get attention.
- Has a few understandable words – e.g., “Mama”, “Byebye”, although they may not be completely clear yet.*
Age: 18 months
Understanding:
- Understands simple questions and follows simple instructions.
- Shows pretend play, particularly using one object as another – e.g., using a shoe like a phone.*
- Turns to look at distant objects other people are looking at.*
Speaking/communication:
- Babbling conversations.
- Points at an object to share interest with another person.*
- Has 3 definite words.*
- May have up to 20 words.
Age: 2 years
Understanding:
- Likes listening to stories.
- Will point to body parts on request.
- Can turn pages in board books.
- Points to pictures they recognise.*
Speaking/communication:
- Words are becoming clearer.
- Uses 2-word sentences - e.g., "Where ball?" "No doggy" "More juice".*
- Uses 50 to 200 words regularly.
Age: 3 years
Understanding:
- Understands 2-stage commands: e.g., "Get your T-shirt and put it in the washing basket."
- Understands contrasting concepts like hot/cold, stop/go.
Speaking/communication:
- Rapid increase in vocabulary.
- 1–3 word sentences.
- Can name 6 body parts.*
- Family can understand them.*
Age: 4 years
Understanding:
- Understands simple "Who," "What," and "Where" questions.
Speaking/communication:
- Can name at least 1 colour.*
- Uses 4 or more words per sentence. Talks about past activities.
- Most people can understand them.
Age: 5 years
Understanding:
- Enjoys stories and can ask simple questions about them.
- Hears and understands everything said to them.
Speaking/communication:
- Speaks clearly and fluently and is easy to understand.*
- Can name at least 4 colours.*
- Uses long, detailed sentences and tells stories.
* describes a communication skill that most children achieve by the age stated.
This table was created using information from the following sources:
- the Ages and Stages Questionnaire (agesandstages.com)
- the Denver II Developmental Screening Test (Frankenburg, Dodds, Archer, Shapiro & Bresnick, Pediatrics, 1992)
- Communication Development | KidsHealth New Zealand's Trusted Voice On Children's Health
Skin infections and skin care
Serious skin infections are one of the main causes of hospital care for babies and young children in New Zealand. The infections can develop when there is a break on the skin that allows germs (bacteria) to enter.
Skin infections can spread from person to person through direct contact with someone with an infection, clothing, used towels, and used bedding. Infections can also enter the body through the eyes, nose, insect bites and cut skin. Scratching untreated eczema is a common cause of skin infections.
Skin reactions from insect bites should be treated to avoid scratching and possible infection.
Keeping skin healthy is important, as it plays an important role in protecting the body and its internal organs from infections. Because a child’s skin is delicate and their immune system is not fully developed, skin infections in babies and young children are common. If these are not treated quickly, the infections can spread and could cause other health problems. Serious skin infections can be prevented by looking after the affected area and getting treatment early.
It is important to clean and cover all sores when they first appear until they are completely healed.
Early signs of skin infection
Early signs of skin infection include:
- an unusual rash, lump, pimple or redness on the skin
- a painful, itchy, open sore that is red and has pus
- a red area that is painful and warm to touch.
Sores can develop anywhere on the body, but the most common parts to be affected are the hands, legs, and trunk (back, chest and abdomen region), of the body and the nappy area.
Take your child to a doctor or nurse if the sore or wound:
- is near the eye
- is on a joint
- has pus
- is warm to touch
- is painful
- is getting bigger
- has red streaks coming from it
- is not getting better after 2 days.
The infection can spread very fast – do not wait for your child to look or feel unwell or have a high fever. Children can get very sick very quickly overnight. They may need antibiotics to stop the infection from spreading.
Common skin infections
The most common types of skin infection are impetigo, boils, cellulitis and scabies.
Impetigo is also called ‘school sores’. The infection usually starts at the site of a minor injury such as a graze, an insect bite, or scratched eczema. Clear blisters or golden yellow crusts may appear, getting bigger and spreading each day. The sores are very itchy. Impetigo is very infectious and is easily passed to other children and adults if they touch or scratch the sores.
Boils are deep infections of the hair follicles and appear as a pimple or one or more tender red spots, lumps or pustules. Large boils form abscesses, where pus is trapped under the skin. Sometimes there may also be cellulitis in the surrounding area (see below).
Cellulitis is an infection that affects a deeper level of the skin. The affected area can be warm, red, tender, swollen, and have streaks coming from it. Children can become generally unwell with fever, chills and shakes. Severe cellulitis may lead to septicaemia (blood poisoning).
Scabies is caused by a tiny insect (mite) that digs under the skin and lays eggs there. Small blisters grow on the skin and get very itchy and can become infected. The scabies rash may start anywhere, but it is usually found between the fingers, on the wrists, around the waist and on the bottom or private parts. Scabies is contagious – if one member of the family has scabies, check everyone else in the family as well.
Keeping skin healthy
Eating healthy food and drinking plenty of water helps to nourish and maintain a healthy skin.
Also keep the skin of children clean and healthy by:
- washing hands often with soap and water
- regular bathing and keeping skin clean and moisturised all the time
- checking and cleaning your baby’s nappy area often
- cutting fingernails and avoiding scratching
- treating eczema and stopping children from scratching it
- cleaning and covering any open skin sores
- checking children’s skin each day
- making sure they wear clean clothes every day
- washing clothes, towels and sheets regularly
- making sure they don’t scratch skin or sores
- treating pets for fleas.
See Skin | KidsHealth NZ for resources about skin and skin infections.
Eczema
Eczema is a common childhood condition that makes the skin itchy, dry, red and sometimes cracked and weeping.
Babies may develop eczema after 6 weeks of age, often on the face and trunk (back, chest and abdomen region) to start with. Toddlers and preschoolers often get patches of eczema around their wrists, elbows, ankles and knees. In severe eczema most of the body surface can be affected.
Eczema can be very different in different people. It can flare up from time to time, with the skin appearing normal in between flare-ups, or it can be fairly constant (chronic). In chronic eczema the skin has patches of dry, itchy and thickened skin, which can be darker or lighter than the skin elsewhere on the body. Skin with eczema gets infected more easily, which can make it painful, weeping and crusted.
Eczema affects about 25 percent of New Zealand children and can affect their quality of life. Fortunately most will grow out of it – only about 2 to 3 percent of adults have eczema.
Eczema is not catching (contagious) but can run in families. Children with eczema are more likely to develop hay fever, asthma and food allergies.
Children who are prone to eczema have skin that is less able to protect the body. This makes them more sensitive to things such as soap, detergents and common chemicals such as chlorine in swimming pools. They may also react to factors like the weather, temperature, dust mites, and other triggers.
Because eczema can be triggered by different things for different children, talk to your nurse or doctor to work out a care plan for managing your child’s eczema. Such a plan might include:
- avoiding soap
- using moisturiser creams (emollients) to moisturise the skin
- using antiseptics (for example, bleach in the bath – for details, ask your Well Child Tamariki Ora provider, nurse or doctor) is often helpful to treat small areas of infection
- using steroid creams to treat active eczema and calm inflammation
- working out what triggers cause the flare-ups, and how to avoid or manage them.
Eczema care needs to be reviewed from time to time to check how well it is working. If the treatment plan is not working, see your doctor or nurse.
Useful websites
Eczema In Children | KidsHealth New Zealand's Trusted Voice On Children's Health has useful information on eczema and how to manage it, including a video clip showing how to apply creams and ointments.
DermNet NZ (click on Dermatitis or Eczema) has information on eczema in babies and young children.
Allergy New Zealand has a very detailed page on eczema.
Looking after your child’s teeth
Children’s teeth are at risk of tooth decay as soon as their teeth begin to break through the gum, usually around the age of 6 months. Tooth decay is largely preventable and preventing tooth decay in young children has major benefits. Cavities in young children’s teeth can cause pain, infection and abscesses that may require antibiotics and possibly even dental treatment under general anaesthetic with hospital admission.
Tooth decay can be prevented by:
- eating a healthy diet that is low in sugar
- avoiding fizzy drinks – fluoridated water and milk are the best drinks for teeth
- not dipping pacifiers or dummies in sugar, honey, or any sweetened drinks
- brushing teeth twice a day with fluoride toothpaste as soon as the first baby teeth start to come through the gum
- having regular dental check-ups from an early age
- avoiding putting your child to bed with a bottle.
Brushing teeth with fluoride toothpaste is very important
You should start brushing the baby teeth as soon as they emerge through the gums. Baby teeth are very important for eating and proper speech. They also save the space for adult teeth and are important for the proper growth of the face and jaw. Use half a pea-sized amount of regular-strength fluoride toothpaste on a small soft-bristled brush and brush twice daily. It is very important to brush children’s teeth before bedtime.
Supervise children when they use toothpaste and make sure they don’t eat it. Use half a pea-sized amount of toothpaste for children under 6, then a pea-sized amount from 6 years of age onwards. Don’t rinse their mouth with water, but teach them to spit out left-over toothpaste. In this way fluoride remains in contact with the teeth for longer and can more effectively prevent tooth decay.
Make sure you look after your own teeth well. Your child will learn most about how to clean their teeth by copying you. Also, your child may catch bacteria from you that can cause tooth decay – for example, by sharing spoons or your toothbrush.
Understanding fluoride labelling
Toothpaste packaging often shows the fluoride content as a percentage, not as parts per million. This table will help you work out how much fluoride a toothpaste contains.
Percentage (%) fluoride is equivalent to ⇒ Parts per million (ppm) fluoride
0.221% sodium fluoride ⇒ 1000 ppm
0.76% sodium monofluorophosphate ⇒ 1000 ppm
0.312% sodium fluoride ⇒ 1450 ppm
Recommended strength at least 1000 ppm fluoride.
Toothache
Contact a dental therapist, dentist, oral health therapist or doctor straight away if:
- your child is in a lot of pain, and/or
- swelling or redness appears on their gum or face, or
- the teeth do not have a normal white appearance.
Teething and toothache
When the teeth break through the surface, the gums will often swell and become tender. When teething, your baby may be restless, cry, drool, have a low-grade temperature, a red cheek, disrupted eating and sleeping patterns, and a desire to bite something hard.
You can ease the symptoms of teething by applying ice cubes wrapped in a wash cloth to the cheek, gently massaging the gums, using a teething ring, or applying a teething gel. It is best to avoid teething rings that have liquid inside, as the liquid may not be safe if the ring breaks.
Teething does not cause serious health problems such as high fever, vomiting, diarrhoea or ear infection. If a child is in a lot of pain, or if there is excessive bleeding, pain, pus in their gums, or swelling in the mouth or face, or the teeth do not have a normal white appearance, contact the Community Oral Health Service 0800 TALK TEETH, 0800 825 583, another oral health professional, or a doctor straight away.
Further information
For more information about your child’s dental health, talk to your doctor, practice nurse, Plunket nurse, or Well Child Tamariki Ora provider, your dentist, or oral health professional.
See It’s Easy to Protect Your Family’s Smile (HE2248) or Free dental care for under 18s – Bee Healthy Regional Dental Service
Other useful websites
Caring for your child's first teeth has a guide to the oral health services available and pamphlets and other resources on oral health.
New Zealand Dental Association | Your Oral Health has a lot of information on oral health for all ages.
Safe drinking water
In the first 6 months, all water for your baby to drink should be boiled and cooled on the day it’s used.
If you are using an automatic kettle to boil water, wait until the kettle switches off.
In cities and towns you can use water from the tap after your baby is 6 months old. It’s fine to use fluoridated water.
If you’re not sure about the quality of the water, boil it. Water from tanks and bore holes should be boiled and cooled for babies and toddlers until they are about 18 months old.
In rural areas, water may contain nitrates, which are dangerous for your baby. It is recommended that the bore owners test their water every five years for chemicals. The local public health unit can help you interpret your test results. Boiling does not remove nitrates and other chemicals.
You can support a safe community for your child
Talk to your local council about safe playgrounds, slow traffic in residential areas, and having fences around:
- edges above banks
- drains (or piped drains)
- streams
- industrial sites.
All domestic swimming pools are required by law to be fenced.
Emergencies – urgent action needed
- Basic life support
- First aid and CPR (rescue breathing and chest compressions)
- CPR for babies under 1 year
- CPR for children over 1 year
- Injury
- Unconsciousness
- Choking (the child may not be able to make any noise)
- Burns
- Poisoning
- Drowning
- Meningitis – a serious infection
- Pneumonia – when coughs and colds get serious
- Asthma
- Broken bones
- Bad cuts
- Diarrhoea and vomiting (upset tummies)
- Fevers and fits
Basic life support
CPR requires you to push hard and fast
DRS ABCD
- D Dangers?
- R Responsive?
- S Send for help
- A Open Airway
- B Normal Breathing?
-
C Start CPR
30 compressions: 2 breaths
If unwilling/unable to perform rescue breaths continue chest compressions
-
D Attach Defibrillator (AED)
as soon as available and follow its prompts
Continue CPR until responsiveness or normal breathing return
This diagram is based on the Basic Life Support Flow Chart developed by the New Zealand Resuscitation Council and Australian Resuscitation Council. For more information see New Zealand Resuscitation Council
First aid and CPR (rescue breathing and chest compressions)
All caregivers should know how to perform CPR. Courses are run locally by Hato Hone St John, Red Cross and other training organisations.
Children and infants who are not responding and not breathing normally will need CPR.
This may happen because the child has a severe illness or a severe injury (including events such as near-drowning, smoke inhalation and electric shock).
What to do first
D - Make sure you yourself are safe. Check for any dangers to yourself such as electricity or traffic.
R - Check responsiveness by calling loudly and shaking the child’s arm.
S - Send for help. Dial 111 and confirm an ambulance is on its way. Do this even if you are alone, before starting CPR.
Open the airway by moving the head into a neutral position and lifting the chin. Do not tilt the head back too far.
If they are not breathing, follow the basic life support sequence.
CPR for babies under 1 year
Use only in an emergency
A
Airway
Open the airway by moving the head into a neutral position and lifting the chin. Do not tilt the head back too far.
B
Breathing
Look and feel for movement of the lower chest and stomach area. Listen and feel for air coming from the nose or mouth.
If they are breathing, place the baby on their side.
C
Chest compressions (CPR)
If the baby is not breathing, start CPR – 30 compressions to 2 breaths.
Put the baby on a firm surface. Place 2 fingers of one hand in the centre of the chest just below the nipples. Push down hard and fast 30 times in about 15 seconds (push down one-third of chest depth).
Once you have completed 30 compressions (pushes) on the chest, breathe into the baby’s mouth 2 times. Seal your lips around the baby’s mouth and nose. Gently puff into the baby until you see their chest rise.
Continue with the cycle of 30 chest compressions and 2 breaths until the ambulance arrives.
CPR for children over 1 year
A
Airway
Open the airway by moving the head into a neutral position and lifting the chin. Do not tilt the head back too far.
B
Breathing
Look and feel for movement of the lower chest and stomach area. Listen and feel for air coming from the nose or mouth.
If they are breathing, place the child in the recovery position.
If you are alone and come across a child over 1 year of age who is not responding and not breathing normally, start CPR immediately (Airway, Breathing, Chest compressions) and then seek help.
C
Chest compressions
If the child is not breathing, start CPR – 30 compressions to 2 breaths.
Put the child on a firm surface. Place the heel of one hand in the centre of the chest just below the nipples. Push down hard and fast 30 times in about 15 seconds (push down one-third of chest depth).
Once you have completed 30 compressions (pushes) on the chest, breathe into the child’s mouth 2 times. Seal your lips around the child’s mouth and nose. You may need to breathe into their mouth and pinch their nose closed. Gently puff into the child until you see their chest rise.
Continue with the cycle of 30 chest compressions and 2 breaths until the ambulance arrives.
D
Defibrillator
Attach a defibrillator (AED) as soon as it arrives. Place the pads according to the diagram on the AED. If paediatric pads are not available, use standard pads. The pads should not touch each other – if they are too large, place one on the front in the centre of the chest and one on the back between the shoulder blades. Turn on AED and follow prompts.
Return to chest compressions and keep going until the child responds or starts breathing normally, or professional help arrives and takes over.
Injury
Dial 111 and ask for an ambulance if your baby or young child has been injured and:
- is, or has been, unconscious (can’t be woken up)
- is being sick or seems sleepy
- has trouble breathing
- has serious burns
- you can’t stop the bleeding
- there is severe pain
- there is bleeding from an ear.
Unconsciousness
If the child is breathing, gently move them onto their front or side so their tongue can’t fall back and stop them breathing.
Stay with them. Watch that they are breathing and not turning blue.
If they are unresponsive and not breathing normally, do CPR.
See CPR for babies under 1 year or CPR for children over 1 year.
Choking (the child may not be able to make any noise)
Babies up to 1 year
If the baby is unconscious, do CPR for babies under 1 year.
If the baby is conscious, follow these steps:
- Call for help.
- Hold the baby down lengthwise on your arm or knee.
- Firmly support the head by holding the jaw.
- Give 5 back slaps between the shoulder blades with the heel of your hand – not too hard – to create an artificial cough.
- If the obstruction still hasn’t come out, turn the baby over face up with head lower than the trunk (or body).
- Give 5 chest compressions in the same place as for CPR, but at a slower rate (1 every 3 seconds).
- Only remove the object if you can see it. Do not try to fish for it as you may push the object down further.
- Continue back slaps and chest thrusts until the object comes out. If the baby becomes unconscious, follow the Basic life support steps and perform CPR for babies under 1 year

[An adult holding a baby down lengthwise on the adult's knee, firmly supporting the baby's head by holding the jaw. The adult is using the heel of their hand to give the baby a back slap between the shoulder blades.]
Children over 1 year
If the child is unconscious, do CPR.
If they are coughing or having difficulty breathing, encourage the child to cough. Do not do anything further at this stage.
If the airway is completely obstructed and the child is conscious but not breathing:
- Call for help.
- Stand to the side of and slightly behind the child. Give up to 5 slaps between the shoulder blades with the heel of your hand, firmly enough to try to clear the obstruction.
- If the obstruction has not come out of their mouth, wrap your arms around the child’s chest and grasp one of your fists with the other hand.
- Give up to 5 quick inward thrusts.
- If the obstruction still has not come out, repeat the sequence of 5 back slaps followed by 5 inward thrusts until the obstruction comes out of their mouth. The aim is to clear the obstruction with each new back slap or chest thrust, rather than necessarily giving all 5.
If the child becomes unconscious, follow the Basic life support steps and perform CPR.
If you can’t remove the object in these ways, do mouth-to-nose (or mouth-to-mouth) breathing on the child until help arrives.

[Steps 2 to 4]
Burns
If your child’s clothing is on fire, STOP, DROP and ROLL.
STOP the child running or walking, as this will fan the flames.
DROP the child to the ground to prevent flames and gases rising towards the head and airway.
ROLL – smother the flames by rolling the child in a woollen or cotton blanket or other non-synthetic material.
Put out any fires.
Send for help.
Ensure a clear airway.
Check that the child is breathing.
Cool the burn area with water continuously over the area for at least 20 minutes. DO NOT use iced water. If the burn area is large, you may need to shorten the cooling period, as cooling a large body area can cause hypothermia in children.
After cooling, the burnt area should preferably be covered with plastic cling film along the limb or body.
If appropriate to do so, elevate the burnt limb to reduce swelling.
Do not burst any blisters that appear.
Do not apply any medications or ointment to the burn.
Get medical help.
Poisoning
Stay calm. Take the product container to the phone if you can.
If the child is awake, call the Poisons Centre on 0800 POISON, 0800 764 766
If the child is sleepy or unconscious, lie them on their side and call 111 for an ambulance.
DO NOT make them vomit without advice from the Poisons Centre or a doctor. Some products (e.g., cleaners) can burn the throat. Vomiting increases the risk of burns and lung damage.
GIVE a small drink of water if the product taken is corrosive or irritating (e.g., household cleaners).
NO OTHER FLUIDS should be given unless advised by the Poisons Centre or a doctor.
Drowning
Call for help.
If the child is not breathing, start CPR immediately they are out of the water.
See also CPR for babies under 1 year or CPR for children over 1 year
Meningitis – a serious infection
If you think your child may have meningitis, contact your doctor, hospital or after-hours medical centre straight away.
What to look for
Not all these symptoms may show at once. Your child may:
- have a fever
- have high-pitched crying or be unsettled
- refuse drinks or feeds
- vomit
- be sleepy or floppy or harder to wake
- have a stiff neck
- dislike bright lights
- have a rash of red or blue spots, or bruising.
Pneumonia – when coughs and colds get serious
Your child with a cough or cold may be in danger and must see a doctor quickly if:
- they are breathing much more quickly than usual, wheezing or making a grunting noise when breathing
- part of the lower chest sucks inward (instead of expanding as normal) as they breathe in
- they are short of breath and cannot drink anything or talk normally.
You can help prevent pneumonia by:
- immunising against the serious diseases on the National Immunisation Schedule
- having a smokefree and vape free home and car
- breastfeeding for at least 6 months.
A child with a cough or cold should have plenty of drinks and can be offered food. If their breathing is normal, coughs and colds will get better. Keep them warm – not hot – and in smokefree and vape free air.
Asthma
Your child with a cough or cold may be in danger and must see a doctor quickly if:
- they are breathing much more quickly than usual, wheezing or making a grunting noise when breathing
- they are putting extra effort into breathing
- the spaces between their ribs are sucked in with each breath
- the spaces above the collar bone are sucked in with each breath.
Asthma often runs in the family/whānau. A child is more likely to have asthma if several people in the family/whānau have it, or have related conditions such as hay fever or eczema.
About one third of all children under 1 in New Zealand will have episodes of wheezing and coughing, especially if they have a cold or are around smokers. Most won’t experience this after about 3, but one quarter of New Zealand children will later prove to have asthma.
Some signs of asthma in children are:
- coughing, particularly at night and after exercise
- breathlessness, often with wheeze
- a tight feeling in the chest.
The main triggers for asthma in babies and toddlers are colds and cigarette smoke.
What you can do to prevent asthma attacks
Ask your doctor for an Asthma Action plan. Use the prevention medication prescribed by your doctor.
Keep your house and car smokefree and vape free. Keep your home warm and dry. Dust regularly with a damp cloth.
Look for things in your home that can cause allergies. Carpets, bedding and sheepskins can hold dust mites, which are known to be triggers for asthma. Wash bedding and soft toys every week.
Pets can also be a trigger, as can some plants in the garden. Pollen is a trigger for some people.
For more information see the resources section of the Asthma Foundation website for booklets, including What Is Asthma, Triggers in Asthma and Children and Asthma.
Broken bones
Don’t move the child unless you have to or are sure you won’t cause pain. Watch them closely. If they cannot be moved, you may need to call an ambulance.
If your child doesn’t need an ambulance, take them to your nearest hospital Emergency Department.
Bad cuts
If there is a lot of bleeding, press hard against the cut with a pad or clean cloth. If there is something stuck in the cut, do not try to remove the object, just press around the cut. Just use your hand if you don’t have a clean cloth. Raising an injured arm or leg (as long as it is not broken) will help stop the bleeding. Get medical help.
Diarrhoea and vomiting (upset tummies)
Diarrhoea can kill babies and children by draining too much liquid from their bodies (dehydration). It is most important to give a child with diarrhoea plenty of drinks. A child has diarrhoea if they have watery, dirty nappies more often than usual.
Signs your child needs medical help quickly
You should get medical help quickly if your child:
- will not drink or eat normally
- has several runny, dirty nappies in 1 or 2 hours
- vomits often
- has a fever
- is very thirsty
- has blood in their nappy
- is unusually irritable
- has sunken eyes and a dry mouth
- has diarrhoea that lasts longer than 24 hours.
IMPORTANT – as soon as diarrhoea starts
As soon as diarrhoea starts, give:
- plenty to drink, to replace the liquid being lost
- light food, if they can keep it down, to keep them nourished.
If breastfeeding, keep feeding more often than usual.
If your child is having formula, give this as usual and other liquids as well, such as:
- water that has been boiled and cooled quickly
- oral rehydration fluid from the pharmacy (Pedialyte or Gastrolyte). No other medicines should be used for diarrhoea, except on medical advice.
Commercial oral rehydration fluids are made to exactly the right formulation and are guaranteed to be sterile.
Give drinks, from a bottle, cup or spoon, every time a child with diarrhoea has a dirty nappy. If the child vomits, wait for 10 minutes and then give small sips often.
Give extra liquids until the diarrhoea has stopped – usually 3 to 5 days.
Do not give sugary drinks, such as fruit juice or fizzy drinks (including flat lemonade). These are dangerous for children who have diarrhoea and can make the diarrhoea worse.
Children over 6 months with diarrhoea can still be given food. Food can help to stop the diarrhoea and keep the child’s strength up.
If your child seems fairly well, but has diarrhoea for longer than 2 weeks, see your doctor.
Preventing diarrhoea
Help prevent diarrhoea by:
- breastfeeding – breast milk is germ-free and safe
- getting your baby immunised with the rotavirus vaccine at the correct times
- cooking food until it is piping hot, storing it covered and cold, keeping everything clean
- everyone washing hands after using the toilet and before touching food or the child – including before and after changing nappies.
If your child is having formula, use it as soon as possible after preparation.
It is important that everything used to make up the formula is very clean. Feeding equipment (including any items used with breast milk) must be washed and sterilised until your child is at least 6 months old and thoroughly washed and rinsed once they are over 6 months. Ask your Well Child Tamariki Ora provider, nurse, doctor or pharmacy for advice about sterilising bottles and teats.
Fevers and fits
Fevers – what to do
Treat fevers by cooling the child and giving them plenty to drink.
To cool a feverish child (even if they are shivering):
- take off clothes and blankets, cool the room and wipe their head and body with a wet, lukewarm cloth (a cold cloth can make them hotter by making the body try to warm up)
- give them plenty of water to drink.
If the child stays very hot and restless, or if their temperature is still rising, keep wiping them with a lukewarm cloth. You can place your hand on the child’s forehead or the back of their neck to feel if they are burning hot, but the best way to know if your child has a fever is to use a thermometer.
A significant fever is when the thermometer shows 38.5°C or above. Digital thermometers give a more accurate reading.
Fits (or convulsions)
Children sometimes have fits when they have a fever. Fits look very scary but usually last only a few minutes.
Short single fits with a fever don’t cause brain damage. One in 20 children have fits with fever – the most likely age is from 6 months to 4 years.
A child having a fit may:
- go stiff and jerk or shake uncontrollably
- become unconscious – not knowing what is going on around them
- have their eyes roll up and breathe noisily and heavily
- vomit, or have froth at their mouth
- clench their teeth tightly
- soil or wet themselves.
Fits – what to do
If the child has a fit, put them on their side and stay with them until it is over.
- You can’t stop a fit once it starts, but you can stop injury.
- Stay with the child. Lie them on their side with face turned so they can dribble out of their mouth.
- Take off any tight clothing around the neck. Help clear air passages by keeping the chin away from the chest if you can.
- Don’t try to jam anything between the gums or teeth.
- Keep the jerking head, arms or legs away from hard things. Make sure the child can’t fall.
If you are beside a telephone, or someone is with you, call a doctor. Otherwise, wait till the fit is over before calling the doctor.
If the fit doesn’t stop after 5 minutes, be sure the child is lying safely, then call the doctor or ambulance – even if you have to leave your child for a few minutes.
When the fit is over
- The child will be sleepy and will probably go into a deep sleep. Don’t try to wake them.
- Clear any vomit from their mouth.
- If they are hot, continue to cool them down. Don’t bundle them up.
- Call the doctor.
Contacts and information
Police/Fire/Ambulance 111
Well Child Tamariki Ora provider Well Child Tamariki Ora providers
PlunketLine 0800 933 922
Healthline 0800 611 116
PlunketLine nurses provide advice on parenting, nutrition, child development and behaviour for children from birth to 5 years.
Healthline nurses and paramedics provide advice on unwell children of any age and health advice for all the family/whānau.
Both services are free and available 24 hours.
National Poisons Centre 0800 POISON (0800 764 766) (24 hours)
Women's Refuge 0800 REFUGE (0800 733 843) (24 hours)
Danger signs
Baby and child sickness
Get help quickly from a doctor if your baby or young child shows any of the signs listed below. Learn CPR (rescue breathing) to be prepared for emergencies.
General
- Cannot be woken or is responding less than usual to what is going on around them.
- Has glazed eyes and is not focusing on anything.
- Seems more floppy, more drowsy, or less alert than usual.
- Has a convulsion or fit.
- Has an unusual cry (high pitched, weak or continuous) for 1 hour or more.
- Has severe abdominal pain.
- Has a bulge in the groin that gets bigger with crying.
Temperature
- Feels too cold or hot (temperature below 35°C or above 38.5°C).
Skin colour and circulation
- Skin is much paler than usual or suddenly goes very white.
- Nails are blue, or big toe is completely white or mottled, or colour does not return to the toe within three seconds of being squeezed.
- Blue colour develops around the mouth.
- A rash develops with reddish-purple spots or bruises – it’s especially important if the spots or bruises don’t disappear when you press a glass onto them.
Breathing
- Struggles to breathe or stops breathing.
- Breathes more quickly than normal or grunts when breathing out.
- Wheezes when breathing out.
Vomiting and diarrhoea
- Has vomited up at least half of their feed (food or milk) after each of the last three feeds.
- Vomit is green.
- Has both vomiting and diarrhoea.
- Has drunk less fluid and has fewer wet nappies or visits to the toilet than usual.
- Has blood in their poo (tūtae).
Emergency numbers
Ambulance/Fire/Police 111
National Poisons Centre 0800 POISON (0800 764 766)
Healthline 0800 611 116
Women's Refuge 0800 REFUGE (0800 733 843)